With all of the testing blunders that have plagued the country’s coronavirus scene, a faster, less-accurate test could be the solution to better controlling the pandemic. Experts are now retracting previous sentiments about the role that rapid tests and a quantity-over-quality strategy could play in bringing back a sense of normalcy.
A rapid antigen test, as the name implies, looks for antigens, foreign substances that elicit the production of antibodies and, in general, an immune response. An antigen test diagnoses active infections by detecting traces of the virus, in this case, the SARS-CoV-2 virus.
On May 9, the U.S. Food and Drug Administration authorized the first antigen test to help in the rapid detection of COVID-19. This test typically produces results in minutes, with the compromise of accuracy due to its lower sensitivity. As of now, the majority of rapid antigen tests are done via a mucous membrane swab.
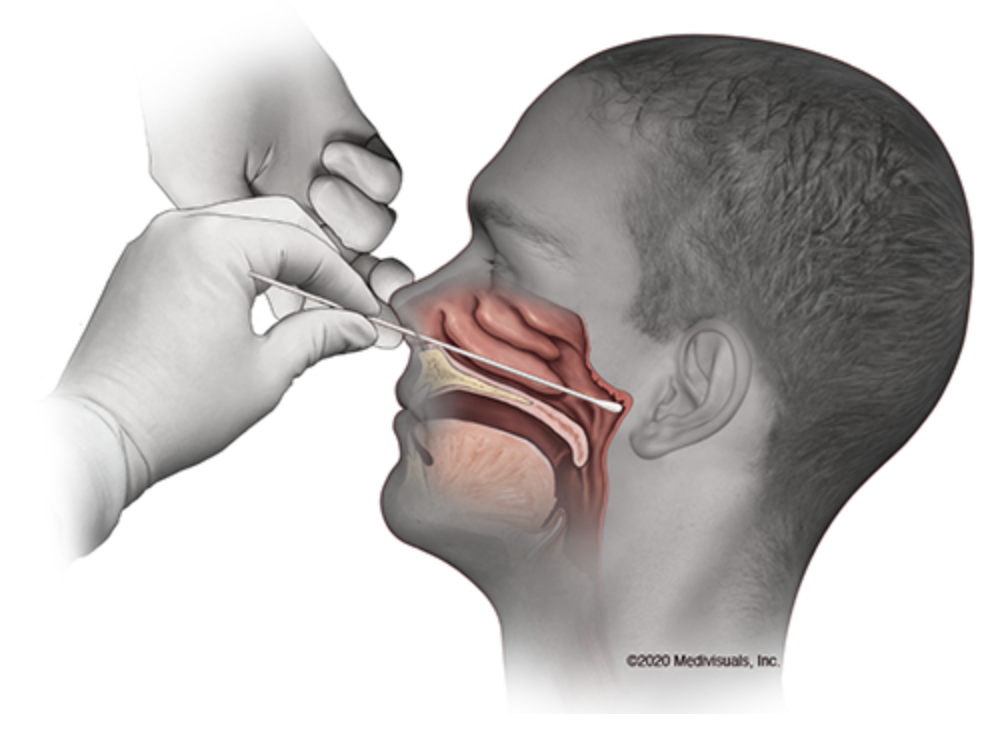
Source: UC Davis Health, MedVisuals
A test that is lower in sensitivity would require a greater viral load, or the amount of virus in an individual, to pick up a positive result. Because of this, rapid antigen tests help communities diagnose the most infected individuals with the goal of mitigating future outbreaks.
“If you have a nursing home and you have residents that haven’t had visitors in months, you could run a rapid test on them. If [the visitor] tests negative, then you can be reasonably confident that they don’t have the virus and you can let them in for a visit,” said Will Humble, former director of the Arizona Department of Health Services and the current executive director for the Arizona Public Health Association.
As of July 30, at least 362,000 people have been infected at nursing homes and other long-term care facilities alongside at least 62,000 deaths from either residents or workers, according to The New York Times. The index case of COVID-19 was in a nursing home in Washington, and ever since then, these facilities have unfortunately seen a plague of coronavirus cases.
RELATED: COVID-19 testing capacity increases with antigen test
In addition to the nursing home setting, rapid antigen tests are useful for employees who need quick results before starting a shift. Although the accuracy is compromised, the fact that the results come in minutes makes the rapid antigen test much more actionable, according to Humble.
“In my opinion, for that kind of setting, that rapid test is superior to the PCR because you get to make a decision on it right away,” Humble added.
Rapid tests have been used in the past, for example, when trying to diagnose cases of the flu on demand. The rapid test for the influenza virus has a sub-optimal test sensitivity, leading to more-than-desired false negatives, especially when influenza activity is high, according to the Centers for Disease Control and Prevention.
“[Rapid antigen tests] can be done within minutes at a doctor’s office, similar to a rapid strep test. They are also much easier and affordable to produce,” said Dr. Natasha Bhuyan, a family medicine physician and faculty at the University of Arizona College of Medicine — Phoenix.
When comparing a rapid antigen test to a PCR test, it boils down to two major factors: level of exposure in the individual and speed versus accuracy. In other words, who are you testing and what is the level of urgency?
If an individual’s level of exposure is high, then a PCR test would be more useful for accurately diagnosing an active infection. However, if the results are pressed for time, then a rapid antigen test could potentially outweigh the need for accuracy.
“Antigen tests play an important role in the overall response against COVID-19, including as a point-of-care test that can potentially scale up to test millions of Americans quickly,” said FDA Commissioner Dr. Stephen Hahn in a press release in July.
RELATED: What is pooled testing and how can it help limit the spread of COVID-19?
With the loss of accuracy in rapid antigen testing, a more widespread approach to testing is undoubtedly needed. If a community isn’t testing enough, then that loss of accuracy is more of a concern. However, Bhuyan noted that the sensitivity of the antigen test has improved since the beginning of the pandemic.
In July, the FDA issued its first emergency authorization for sample pooling in diagnostic testing, so the test-four-in-one strategy would help get more bang for your buck. With pooled testing now in play, rapid antigen testing has become more widely discussed.
A study published in the Journal of the American Medical Association looked at speed versus accuracy for coronavirus tests. The study, published on July 31, came to the conclusion that a more insensitive test that is used more frequently is more beneficial than an accurate test that is used less often.
“In this modeling study, symptom-based screening alone was not sufficient to contain an outbreak, and the safe reopening of campuses in fall 2020 may require screening every 2 days, uncompromising vigilance, and continuous attention to good prevention practices,” the authors wrote.
The researchers found that the frequent screening, meaning every two days, of all students with a low-sensitivity and high-specificity test — like the rapid antigen test — might be required to control outbreaks at a justifiable cost.
These tests could be done at a doctor’s office or even at home at a cost of a few dollars. Some experts even estimate these tests could cost as little as $1 or less.
“Even if someone has negative antigen or PCR results, they need to continue to stay at home when they can, wear a mask when they are around others not in their household, physically distance, and practice good hand hygiene. Ultimately, it’s those steps that will really help reduce the transmission of COVID-19,” Bhuyan added.
As universities and other schools around the country begin to open, a quantity-over-quality approach to testing could be the best way to mitigate the spread of the virus and reduce the risk of overwhelming the U.S. hospital system, similar to what happened in March.
Follow Amit Syal on Twitter









