Editor’s Note: On the evening of Thursday, Aug. 27, CDC director Dr. Robert Redfield aimed to clarify earlier guidance, saying that “testing may be considered for all close contacts of confirmed or probable COVID-19 patients.”
On Friday, Sept. 18, the CDC noted that “due to the significance of asymptomatic and pre-symptomatic transmission, this guidance further reinforces the need to test asymptomatic persons, including close contacts of a person with documented SARS-CoV-2 infection.”
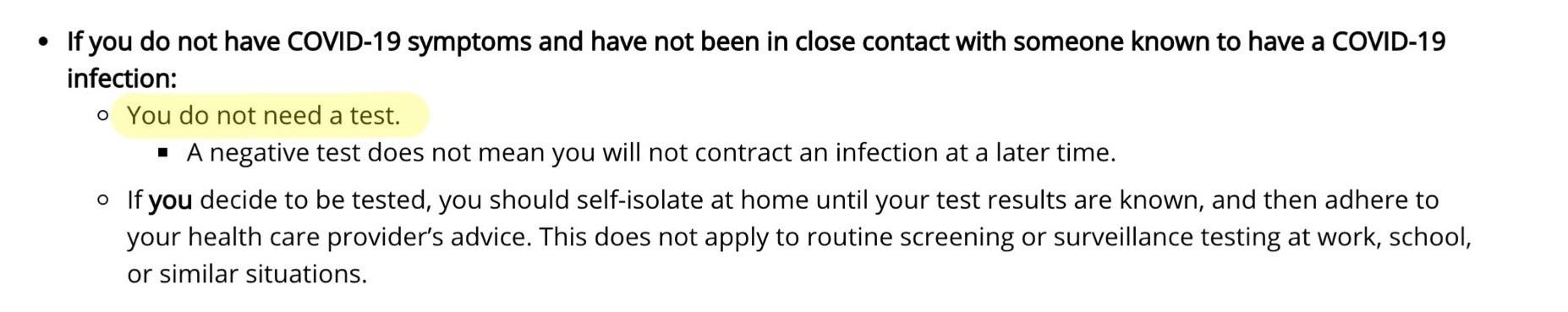
Earlier this week, the Centers for Disease Control and Prevention modified its guidance regarding who to test for COVID-19 — a move that has sparked controversy from those in the scientific community. The agency said that people who are asymptomatic do not need to be tested for COVID-19 when that cohort of infected individuals make up nearly half of those who are infected, according to that same agency.
Arguably two of the greatest tools we currently have when it comes to fighting the pandemic are the use of masks in public spaces and widespread and frequent testing. However, limiting testing to only those individuals with symptoms defeats the purpose of proactively trying to mitigate future outbreaks.
Earlier in August, the National Institutes of Health launched the Rapid Acceleration of Diagnostics initiative to speed the innovation of the development and implementation for COVID-19 testing technology. The federal program advocated that “testing must also be inexpensive, user friendly, widely accessible in a variety of settings and locations, and able to detect people who are asymptomatic.”
However, this new CDC guidance undermines that call-to-action from the NIH to test a more widespread group of individuals and help control the spread of the coronavirus.
“It seems to be a big mystery to all of us,” said Purnima Madhivanan, a physician and epidemiologist at the Mel and Enid Zuckerman College of Public Health. “This particular change in the CDC guidelines is very, very concerning.”
RELATED: ‘No celebration, no victory lap. We’re going to stay the course’: The story of Arizona’s 180
The idea of being asymptomatic is a double-edged sword. On a personal level, not having a sore throat, fever or cough, among other symptoms, might be a plus. However, from a public health standpoint, asymptomatic carriers will continue to leave the house and unknowingly contribute to the spread of the virus. The lack of visible symptoms in these individuals makes it hard to isolate and remove them from circulation.
Madhivanan believes this change in guidance is “unacceptable” because the evidence indicates that asymptomatic carriers of the virus make up a very large percentage of those infected with the coronavirus. Identifying asymptomatic carriers of the virus is critical not only for identifying the contacts, but also in terms of isolation and mitigation measures, she said.
“We need to have a public health response, and we cannot have that if we don’t know what is going on in our community,” Madhivanan said. “I think one of the challenges we are having is that a lot of the decisions right now are not science and evidence-driven. … We need to start focusing our decision on scientific evidence.”
Without more frequent testing — especially with those who do not present with visible signs and symptoms — getting a better grip on the pandemic becomes all the more difficult, even more so in a time when students all across the nation are starting to return to class, both virtually and in-person.
UPDATE: On Sept. 18, the CDC updated its previous guidelines about who test for COVID-19. The agency says that if you have been in close contact with a person who has a document SARS-CoV-2 infection for at least 15 minutes, then “you need a test.”
Follow Amit Syal on Twitter









