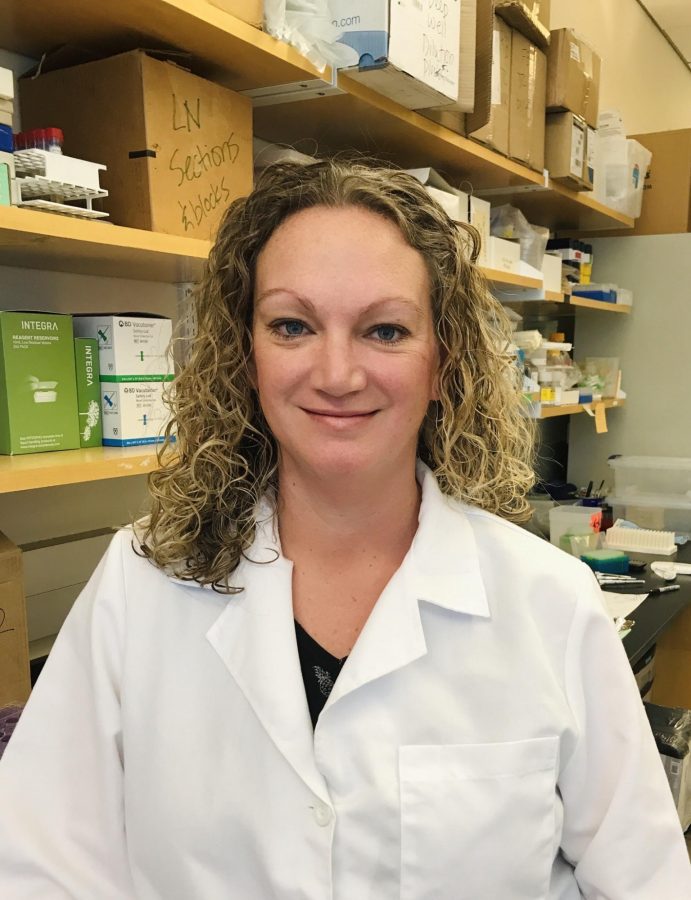
A University of Arizona coronavirus researcher, Jennifer Uhrlaub, never expected to fall ill to the virus until she tested positive on June 15.
Uhrlaub suspects she was exposed to the virus when she visited her local grocery store before going on a road trip with her family to Nebraska. She was going to visit her husband’s family and both families thought it was a low risk to spend the week together. However, symptoms began to show and spread between the extended family members.
Her husband was the first person to have symptoms and they assume he was the first person infected. Uhrlaub and her husband used his debit card receipts to determine that they were most likely exposed to the coronavirus at the grocery store.
“The irony is that he had been working from home the entire time and had very few trips anywhere,” Uhrlaub said in an email.
Uhrlaub’s symptoms lasted about a week and she reported having headaches, chills, body aches, a very mild cough, fatigue and a loss of taste.
“I think I’m fortunate that my case of [COVID-19] was mild and that no one in our family required hospitalization,” Uhrlaub said in an email. “I still worry about long term consequences, there is so much we don’t know about what this virus can do.”
She explained how knowing the range of symptoms and potential for serious complications made her anxiety the worst part of her experience. Some of the family members that were infected mainly interacted with Uhrlaub and her family outside on a very windy afternoon and they still became infected.
“I knew the virus was very contagious before we got it but experiencing it really drove that point home,” Uhrlaub stated.
RELATED: Three-day spike accounts for 75% of University of Arizona positive coronavirus tests
Uhrlaub explained that after she and her family were together Sunday afternoon, her husband developed symptoms that evening and immediately separated from the rest of the family that night. Her husband and she were then tested on Monday. Her positive result was reported on Wednesday and she didn’t have a single symptom until Thursday evening.
“It really does happen that you can spread it to those you love with no hint that you are sick,” Uhrlaub stated.
Urlaub’s role in the development of the university’s antibody test was to validate the high-throughput enzyme-linked immunosorbent assay, which recently received the U.S. Food and Drug Administration’s approval, against a plaque reduction neutralizing test. The plaque reduction neutralizing test uses live SARS-CoV-2 and must be conducted in a Biosafety Level 3 laboratory.
“For this reason, it is not an assay that can be run on every patient sample. Instead, we compared results from the ELISA to those of the PRNT and ensured that if a person was scored as positive on the ELISA that their serum would also neutralize live virus,” Uhrlaub said in an email.
Uhralub explained that this means if a person has their antibody test and is told they are positive, then they have antibodies that are capable of neutralizing the virus. Their test also has a very low false-positive rate.
“This is important when the population of people you are sampling includes only a small percentage of people who have been infected,” Uhrlaub said in an email.
Uhrlaub and others she has trained will be running more neutralizing antibody tests in support of a $7.7 million grant to Dr. Jeff Burgess from the U.S. Centers for Disease Control and Prevention. She is also working with a team of faculty across multiple departments at the UA to develop mouse models of COVID-19.
“Hopefully, we will have a licensed vaccine soon. This is the tool we really need to achieve our new normal,” Uhrlaub stated.
Follow Jillian Bartsch on Twitter