Dr. Christian Bime is a pulmonary and critical care physician who has been working on the front lines since the inception of the COVID-19 pandemic. After finishing a fellowship in pulmonary and critical care medicine from the Johns Hopkins University School of Medicine in 2013, Bime started working at Banner University Medical Center — Tucson.
According to the Arizona Department of Health Services, roughly 9% of the total confirmed cases of COVID-19 have resulted in hospitalizations. For the past few months, Bime has spent pretty much all his time at work seeing COVID-19 patients in the intensive care unit.
Patients who are sent to the intensive care unit for COVID-19 typically have respiratory failure, among other critical problems. They could potentially require mechanical ventilation, dialysis for kidney failure or medications to combat low blood pressure as a result of septic shock, a life-threatening infection that can spread throughout the body and cause respiratory and heart failure, dangerously low blood pressure or even death.
When seeing his patients, which can be upwards of 40 per day, Bime has to wear personal protective equipment to avoid getting himself infected from the virus. A typical outfit for Bime includes a gown, gloves, a face shield and an N95 mask, which is sometimes doubled up with an extra surgical mask on top.
“Each time you go into a room to see a patient you have to wear all the personal protective equipment, or PPE. When you come out of the room, all of the disposables need to be removed and thrown away,” Bime said. “PPE that is not disposable, like the face shields, have to be wiped clean with disinfecting wipes.”
RELATED: How does COVID-19 manifest and what can you do if you begin to show symptoms?
After the Food and Drug Administration gave an emergency use authorization for the antiviral drug remdesivir on May 1, Bime said he has been using the drug on some patients depending on if they meet the requirements, they qualify for it and, of course, if its supply can meet the demand.
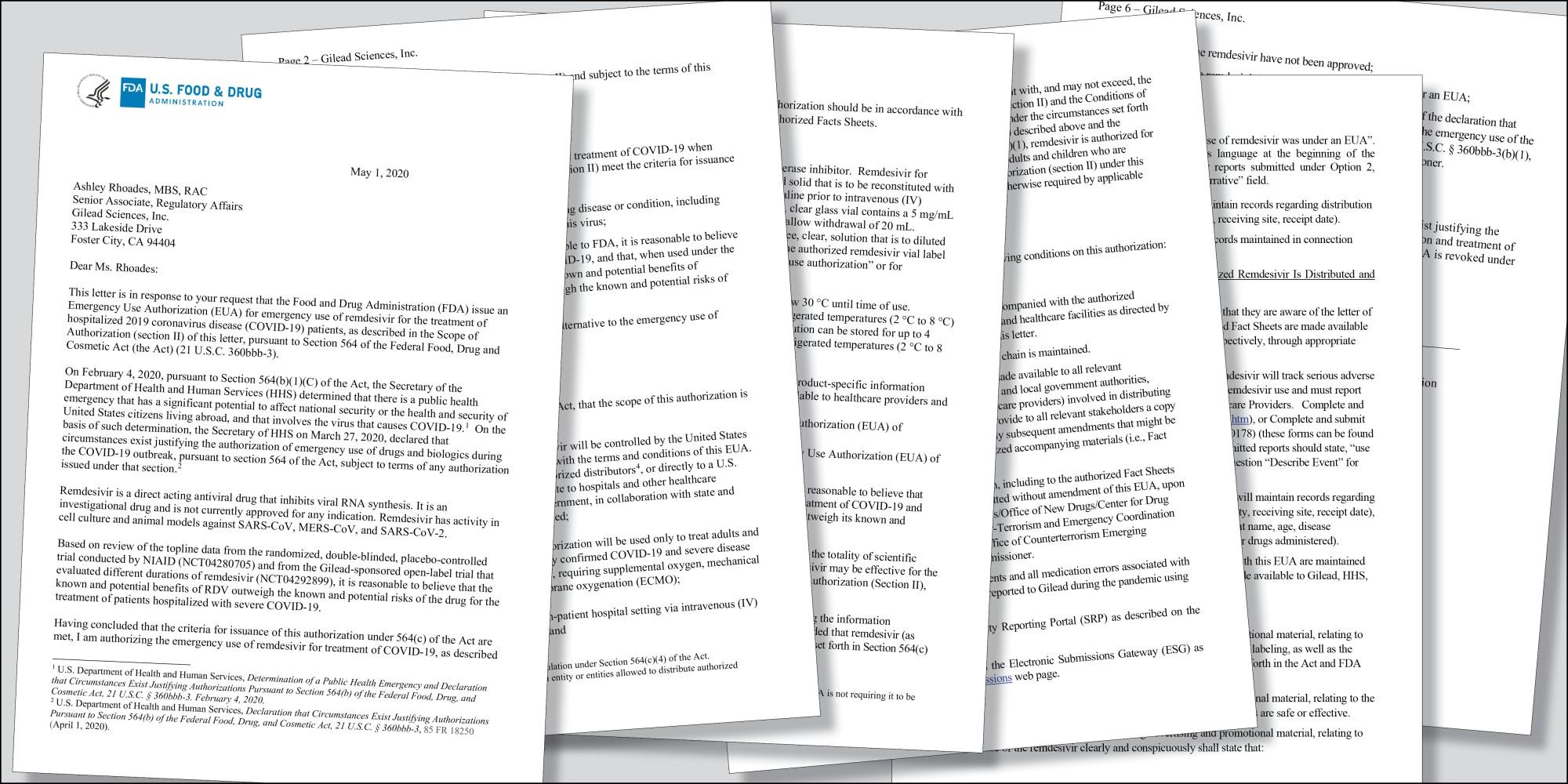
The letter from the chief scientist at the FDA wrote, “there is a public health emergency that has a significant potential to affect national security or the health and security of United States citizens living abroad.”
The emergency use authorization went on to say that the “potential benefits of [remdesivir] outweigh the known and potential risks of the drug for the treatment of patients hospitalized with severe COVID-19.”
However, new research out of the United Kingdom recently indicated that the steroid dexamethasone could make a difference in treating patients with severe COVID-19 illnesses by suppressing inflammation. In the midst of a troubling past few months, this steroid could be a difference-maker but was originally criticized for the lack of transparency about releasing the original research manuscript associated with the study.
“The thought is that by blunting the inflammatory response, we can reduce the severity of severe respiratory failure in patients with COVID-19,” Bime said. “We will need to have confirmation from subsequent studies that dexamethasone is indeed a game-changer for COVID-19 respiratory failure.”
A common complication in patients with a severe COVID-19 illness is acute respiratory distress syndrome, which, according to Bime, is a severe inflammatory response of the lungs that can lead to respiratory failure and multiple organ dysfunction syndrome.
Before the pandemic struck, Bime would still see patients in the ICU but in a much different capacity and with a very different level of stress.
“Under normal circumstances, if we have 20 to 30 patients in an adult ICU, four or five patients might have very severe refractory respiratory failure,” Bime said. “Now, it’s nearly 100% of patients.”
When the pandemic hit, it was a shock for many reasons, but namely, because the SARS-CoV-2 virus is new and can often be enigmatic in its behaviors. Researchers across the globe are working to develop more antivirals and eventually a vaccine as a means to create herd immunity in the population.
RELATED: What is herd immunity and can it help mitigate the spread of COVID-19?
It’s no secret that COVID-19 has been a burden on hospitals around the country, but Bime says his home life was “significantly” affected by the pandemic.
“I had to quarantine myself from my family,” he said. “Luckily I had a section in my home where I could literally be separate from everyone else. I would shower, go to work, come back, say hello from my phone to everyone else.”
In the first week, Bime would eat his meals — along with everything else — away from his family, but soon after, he realized that after a shower to clean himself, he could afford to sit at the dinner table with them and spend time after being at work for so long.
“It’s a learning process,” Bime said.
With everything going on in the world right now and with healthcare workers on the front lines, they are often called “unsung heroes” by many. In New York City, the epicenter of the pandemic for a while, a 7 p.m. applause for healthcare workers became a regular occurrence through the worst of it.
“I got into medicine because of a dedication to serve,” Bime said. “I do not fancy myself a hero. I just feel that this is an opportunity to step up and serve. Hero? Probably not, because I’m simply doing the things I do every day.”
As many know, the road toward becoming a physician is long. After college, aspiring doctors attend medical school for at least four years combined with three to seven years as a resident physician in training, depending on the specialty. After this, some physicians opt for a fellowship that can add a few extra years. Did Bime’s extensive experience as a student and physician-in-training truly help him prepare for unprecedented times like these?
“Yes,” he explained. “Especially my training in critical care medicine. There’s just something about critical care training that prepares you for emergency situations. In essence, that’s what we do every day.”
As expected after lifting a stay-at-home order, cases in Arizona have increased. However, a bit more concerning is the spike in cases Arizona has been experiencing throughout the past few weeks. On June 18, Arizona saw an increase in 2,519 confirmed cases and a day later, 3,246 new confirmed cases.
RELATED: Arizona sees increased ICU usage, upward trend of COVID-19 cases
“If it was just [due to increased] testing, we would not see an increase in the number of people who are coming in sick to the hospital and to the ICU,” Bime said.
As someone who has been on the front lines treating patients on a daily basis, Bime recognizes the severity of the pandemic and encourages everyone to continue following the guidelines despite a longing to return to the “normal” we all had before the pandemic struck.
“COVID-19 is real,” he said. “It is not a hoax. It will be with us for a long time, so we have to adapt ourselves to live with this virus. This is a new normal.”
Follow Amit Syal on Twitter