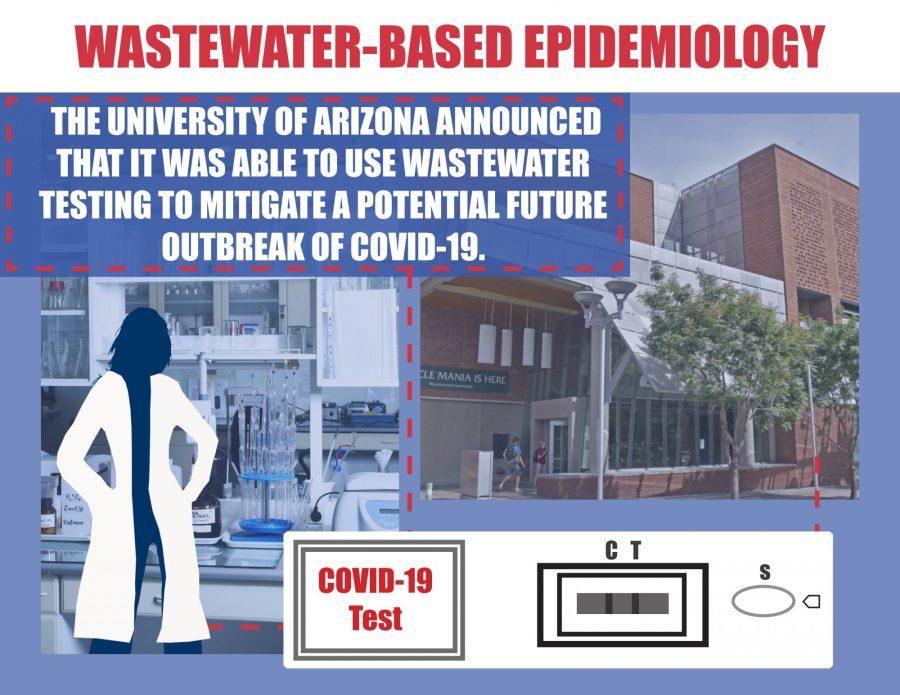
Last week, to the surprise of many around the country, the University of Arizona announced that it was able to use wastewater testing to mitigate a potential future outbreak of COVID-19. When a sample of wastewater came back positive from the Likins Residence Hall, the UA tested all of the dorm’s 311 residents and found two asymptomatic students who tested positive and were immediately quarantined.
“With this early detection, we jumped on it right away, tested those youngsters and got them the appropriate isolation where they needed to be,” said Richard Carmona, a former U.S. surgeon general who also leads the UA’s reentry task force, last week in a briefing.
RELATED: Campus reentry update: Task force discusses early detection of potential outbreak in Likins dorm
Wastewater-based epidemiology is a strategy that has been used for decades to detect traces of a virus in sewage, which has a significant benefit of being a leading indicator of who is infected, according to Ian Pepper, the director of the University of Arizona’s Water and Energy Sustainable Technology Center and one of the leaders behind UA’s wastewater-based testing strategy for COVID-19.
“The idea behind wastewater-based epidemiology is that if someone is infected, they shed the virus and it ends up in the wastewater in the sewer line,” Pepper said. “By testing the wastewater, we get an indication of the total virus load coming from that particular dormitory. We can come up with a quantifiable number of gene copies per liter, and from that, we can gauge how intense the infection rate is in the dorm.”
Once the sewage sample came back positive last week, officials at the university used both antigen and PCR tests to identify the infected individuals and put them in quarantine to mitigate a potential future outbreak. However, one of the biggest benefits of wastewater-based epidemiology, Pepper emphasized, is the fact that it gives the university a leading indicator of who is infected.
RELATED: What’s in a good coronavirus test, accuracy or speed? It depends…
“When someone gets infected, they start shedding the virus right away, whereas it may take 7-10 days before they develop symptoms,” Pepper added. “So you have seven precious days to intervene, and that’s exactly what we did last week in Likins Hall … It couldn’t have gone any better, really.”
Pepper noted that the following day, after the two asymptomatic infected individuals were moved to Babcock Residence Hall, the sewage sample from Likins tested negative, deeming their efforts a success. Without the wastewater-based testing, those two students likely would not have been tested until they either developed symptoms, at which point they would have been in contact with dozens of other students.
“So we think this is going to be a very valuable tool to help us get out in front,” said UA President Dr. Robert C. Robbins in a weekly briefing. “What we really need to find out is who are the people who are asymptomatic that are positive.”
After seeing the success on campus, other universities across the country have called Pepper and his team to get help with the process of wastewater-based epidemiology. The UA is also working on expanding their wastewater-based epidemiology efforts to more locations on campus, Pepper noted.
The samples are discolored water that contains a mixture of urine, fecal matter and water that go through the pipes at the on-campus residence halls. Initial samples are collected around 8:30 a.m. after students have gone to the bathroom and then are sent over to the WEST Center.
From there, sample prep takes an additional couple of hours before doing the extractions which takes a few more hours. Finally, the team does both reverse transcriptase PCR (RT-PCR) and quantitative PCR before the results come in around 5 p.m.
Wastewater-based epidemiology is not a new strategy, but it has been at the forefront of more discussions recently, given the emergent public health crisis this year.
“It started 20 years ago for the poliovirus, but interestingly not a lot was done between. However, this process can be done for any infectious virus,” Pepper said. “Really what we’ve seen is an explosion of wastewater-based epidemiology all over the world, in Australia, Japan and Europe, you name it.”
The UA is starting its second week of classes and, as of Aug. 28, has a total of 65 confirmed positive antigen tests. Other universities that went in with the mindset of a hybrid model of instruction, like the University of North Carolina at Chapel Hill, have had to swiftly transition to remote learning after a number of different coronavirus clusters all across campus.
“It definitely makes the transition [to online classes] easier, and so far, we’re doing a lot better than a lot of other schools,” Pepper said.
Follow Amit Syal on Twitter