A pair of surgeons at the University Medical Center has developed a groundbreaking medical procedure that could save victims of a pancreatic disease from developing severe diabetes.
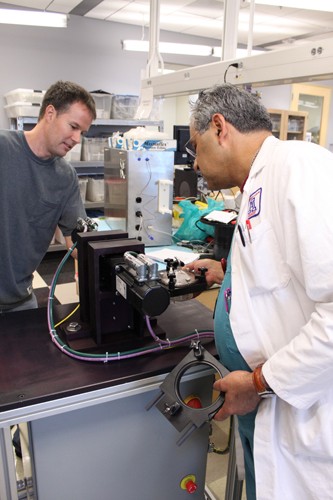
Horacio Rilo, M.D., director of the Center for Cellular Transplantation and Rainer Gruessner, M.D., chairman of the UA Department of Surgery, are the lead developers of the procedure, known as “”auto-islet cell transplantation,”” for patients with severe chronic pancreatitis, a disease of the pancreas that can lead to cancer.
The pain caused by pancreatitis can be severely debilitating, Gruessner said, adding, “”Once you are diagnosed with pancreatic cancer, you are pretty much dead.””
In the past, the common treatment for pancreatitis is to remove the pancreas completely to alleviate pain and prevent cancer. However, the removal of the organ also removes the islets inside the pancreas that produce insulin. Without these islets, patients develop a severe form of diabetes, known as brittle diabetes, and are dependent on insulin for the rest of their lives.
Brittle diabetes is the most extreme type of diabetes and comes with many other problems, Gruessner said, including heart disease, blindness, stroke and early death.
Rilo and Gruessner have developed an operation where the pancreas is removed but islets are transplanted into the liver, making the diabetes less severe. In the best-case scenario, patients can become independent of insulin. In the worst-case scenario, they need only a small number of units of insulin daily.
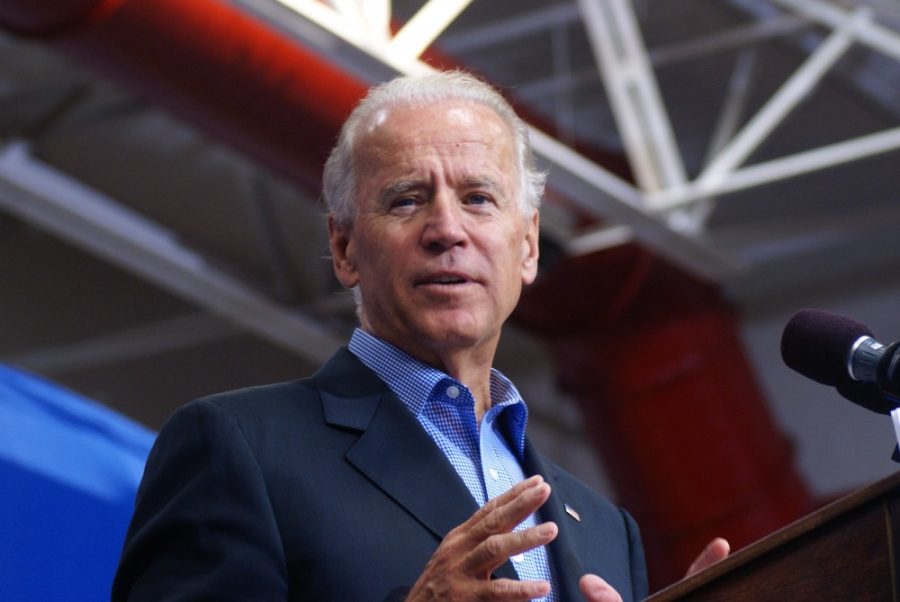
Only a handful of people in the world can perform this surgery, Gruessner said. He said he was able to procure $1.5 million from UMC to develop state-of-the-art facilities and sign on Rilo to assist in the actual surgery.
“”Without the recruitment of Dr. Rilo,”” Gruessner said, “”these life-changing surgeries would not be possible.””
The surgeons have performed two islet cell transplants so far, out of 1,500 to 2,000 potential patients.
In the procedure, the pancreas is removed, then the islets — which make up about two percent of the pancreas — are separated from the pancreas and implanted in the liver.
Rilo said he had to build his own equipment to make the isolation possible.
“”It’s not like I can go to a store and say I’d like one of those and one of those,”” he said. “”No one else in the world is doing this. I have to build everything from scratch.””
Rilo’s lab is filled with new technologies and exciting discoveries, said Jo Marie Gellerman, public affairs official for the UMC.
“”Dr. Rilo is the ideal mad scientist,”” she said.
Robots and high-tech isolation machines are among the tools Rilo has built to make the isolation successful. He has a room in his lab — known around the lab as “”Brain Box”” — that contains different pieces of equipment he is working on, things that have been momentarily discarded, and inventions waiting to happen.
“”We use anything we can to make what we need. Salad bowls from Target — and Martha Stewart, of course,”” Rilo said.
The next step in the development of this technique, Gruessner said, is using islet isolation and transplant to reverse diabetes. Rilo and his team are already making skin for burn victims, liver cells for liver operations and working with transparent fish to watch the internal operations that allow them to swim.
“”What we do here is regenerative medicine,”” he said. “”You can’t wait until an organ fails. Then it is too late.””