The past few weeks have seen an increasing number of developments regarding COVID-19. What started out as a disease limited to one country has made its way to at least 185 countries around the globe.
As of April 26, the U.S. has nearly 1 million confirmed cases of COVID-19 alongside 55,000 confirmed deaths. Due for the development of antibody tests, researchers and scientists have been able to discover that the real number of infections trumps the current confirmed number by an overwhelming amount.
A recent study from the University of Southern California found that the penetrance for the disease in L.A. County could be 28 to 55 times higher than the reported amount, meaning that the disease is significantly less deadly than previously thought. The current death rate in the U.S. falls around 5%, but it is most likely a lot lower given the under-reported number of infections.
RELATED: What are the different tests for COVID-19 and how do they work?
A significant drawback of using the antibody test on a population that is not severely affected is that the rate of false positives can sometimes mirror the rate of true positives. Take a sample population of 100 people where the infection rate is 5%, meaning that five of the 100 people are actually infected.
Now consider a test with a 95% chance of correctly identifying people who lack those antibodies. That sounds amazing, but in a situation where only 5% of the population is infected, the 95% rate can actually be very costly. In that same sample population, five of the 100 people will get a true positive result, meaning that they really do have antibodies.
However, five of the 100 people will also get false positives, meaning that they are falsely reassured. That means that out of the 10 total positive test results, only five, or 50%, are true positives. 50% of the people who tested positive have a false sense of confidence, which can be detrimental in terms of how they behave with that false reassurance.
Antibody tests with a 95% chance of correctly identifying people who lack those antibodies work better when the rate of infection is a lot higher, meaning that as the disease progresses and infects more people, these tests will only become more important.
RELATED: How does COVID-19 manifest and what can you do if you begin to show symptoms?
A new report by the Centers for Disease Control has indicated that certain minority groups, namely non-Hispanic blacks, are disproportionately affected by COVID-19.
As of April 18, non-Hispanic blacks comprised 31.4% of overall COVID-19 hospitalizations in the U.S. Meanwhile, this same minority group only comprises roughly 13% of the U.S. population, according to the most recent U.S. Census. That’s alarming. But what makes this minority group so susceptible to having a severe infection?
A key reason for this is the fact that blacks have proportionally higher rates of underlying health conditions, including hypertension, heart disease, and diabetes, to name a few.
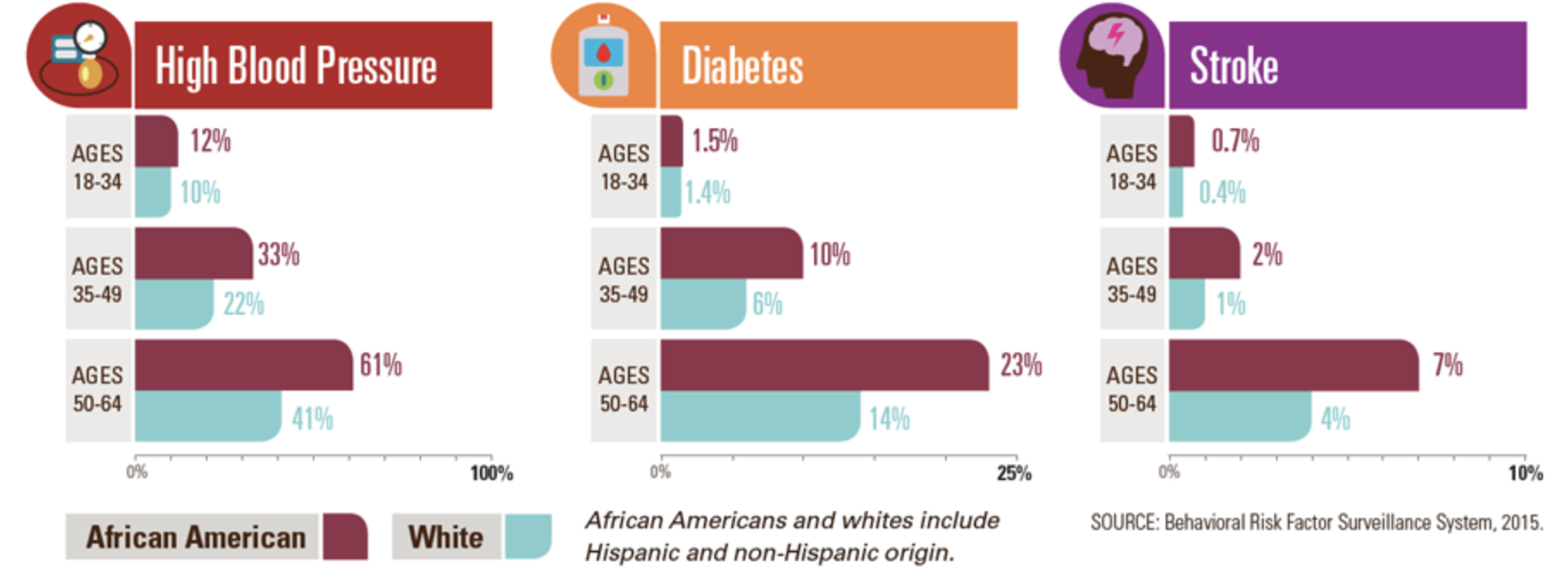
Source: CDC
When a person has an underlying health conditions, their bodies are not as “well-equipped” to fight off the virus as someone without any underlying health conditions. Their immune system becomes a lot more strained fighting the virus and as a result, they often experience worse symptoms and are forced to be hospitalized.
We’ve all heard the idea that those with underlying health conditions are more susceptible to succumbing to COVID-19, but that’s a real-life, prevalent and current example of it.
Another factor that exacerbates the health disparities in the U.S. is the fact that blacks are more likely to be uninsured compared to their white counterparts.
As of 2018, the uninsured rate among African Americans was 9.7%, while it was nearly half of that (at 5.4%) among whites, according to the U.S. Census. Without health insurance, treating a severe COVID-19 infection becomes all the more difficult and puts African Americans at a much greater risk for dying from an infection.
A recent study by the Economic Policy Institute showed that from 2017 to 2018, 19.7% of black or African American workers could work from home compared to 29.9% of white workers and 37% of Asian workers who could do so. When a worker holds an “essential” job and is unable to work from home, they become more likely to contract the virus and fall ill.
A predisposition to underlying health conditions combined with less access to healthcare and an inability to work from home has exaggerated the health disparities that have existed in the U.S. for so long. In the state of Arizona, a similar health disparity exists among the Native American population. For a group that makes up about 5% of the state’s population, they account for 20% of the deaths related to COVID-19.
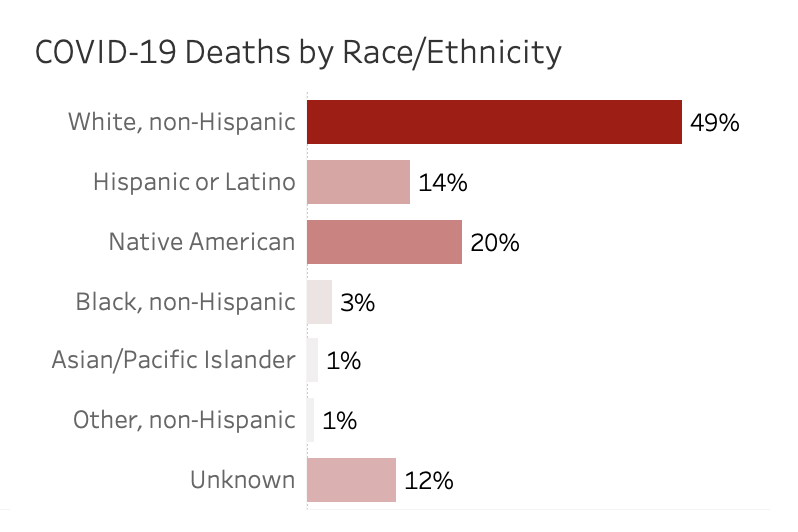
Source: Arizona Department of Health Services
Native Americans have been hit hard by the novel coronavirus for a lot of the same reasons as blacks. A high percentage of underlying health conditions combined with less access to healthcare and treatment puts them in a tough situation.
According to the Indian Health Service, “American Indians and Alaska Natives continue to die at higher rates than other Americans in many categories, including chronic liver disease and cirrhosis, diabetes mellitus, unintentional injuries, assault/homicide, intentional self-harm/suicide, and chronic lower respiratory diseases.”
As the spread of the novel coronavirus progresses, the long-standing healthcare disparities in the U.S. will continue to be brought to light.
RELATED: Online classes: a protective measure to flatten the curve
In total, the state of Arizona has just over 6,500 confirmed cases of COVID-19 and 275 confirmed deaths, as of April 26. The state has about 1700 total ventilators, but only 28% of them, or 482, are in currently in use, as of April 24. Of the 482 total ventilators being used, 191 are being used for COVID-19 purposes, according to the Arizona Department of Health Services.
With a potential re-opening on the horizon, testing is absolutely essential to monitor the spread of the virus. As of April 25, about 63,000 total tests for COVID-19 have been completed in Arizona with 8.7% of them coming back as positive. For now, continue to practice responsible social distancing and keep up to date with CDC guidelines regarding the spread of the novel coronavirus.
Follow Amit Syal on Twitter