Last week, The Daily Wildcat put up a poll on Instagram asking what its followers would like to know about the ongoing COVID-19 pandemic. Here are the top five questions and their answers.
Question: What makes this virus any different from H1N1 or Ebola. How is it worse?
Daily Wildcat: The novel coronavirus, SARS-CoV-2, has a number of differences compared to H1N1 or Ebola. For starters, this novel strain is more contagious than either H1N1 or Ebola.
When dealing with diseases, R0 (R naught) is a value that indicates for every person infected, how many other are likely to become infected just from that original individual. Experts typically place the R0 for SARS-CoV-2 between 2-3, meaning that for every person infected with it, two to three others will likely become infected.
The R0 value for H1N1, also called swine flu, was between 1.4 and 1.6, which may not seem markedly different. However, a small change in a R0 value can make a great difference over time. Ebola, similar to HIV, is a disease that is transmitted through bodily fluids, and so they are not as easily spread as respiratory illnesses. Experts typically place the R0 value for Ebola between 1.5 and 2.0.
The Centers of Disease Control estimates that there were 60.8 million cases of swine flu, with nearly 12,500 deaths in the U.S., giving it a fatality rate of about 0.02%. Although the fatality rate of COVID-19 has fluctuated a lot, it is undoubtedly a lot higher than 0.02%. Current estimates typically place it in the 1-4% range.
If you’re curious about how the COVID-19 pandemic stacks up against some other ones, check out the story down below from a couple of weeks ago.
Q: When does the Wildcat estimate the virus being over?
DW: The Wildcat has no estimates for when the virus will “be over.” But, until a vaccine is produced and readily available to the public, it will very difficult to control the spread of the novel coronavirus. So, hopefully the people you are quarantining with aren’t that bad to constantly be around.
RELATED: Is a vaccine the silver lining of the COVID-19 pandemic?
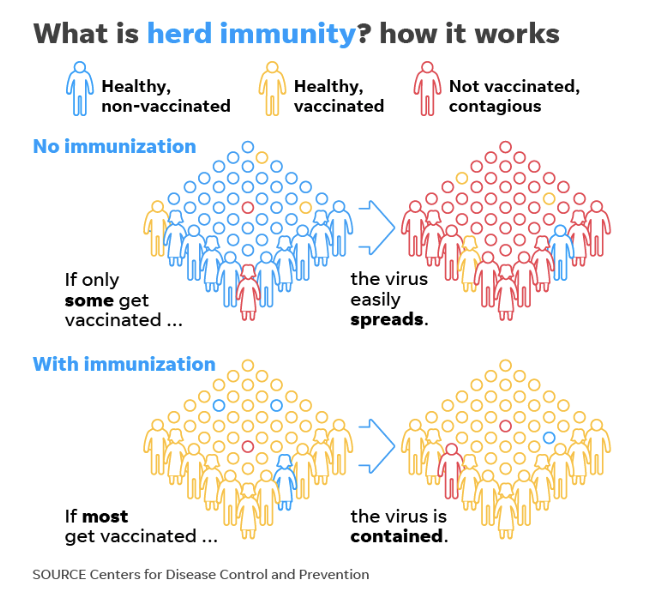
Source: CDC
Q: How likely is it for an average person to get the virus?
DW: Since you’re an expert on R0 values now, you can guess the odds of becoming infected aren’t that low anymore. Just to reiterate, for every person infected with the novel strain of coronavirus, two to three people will likely also become infected. That has exponential growth written all over it.
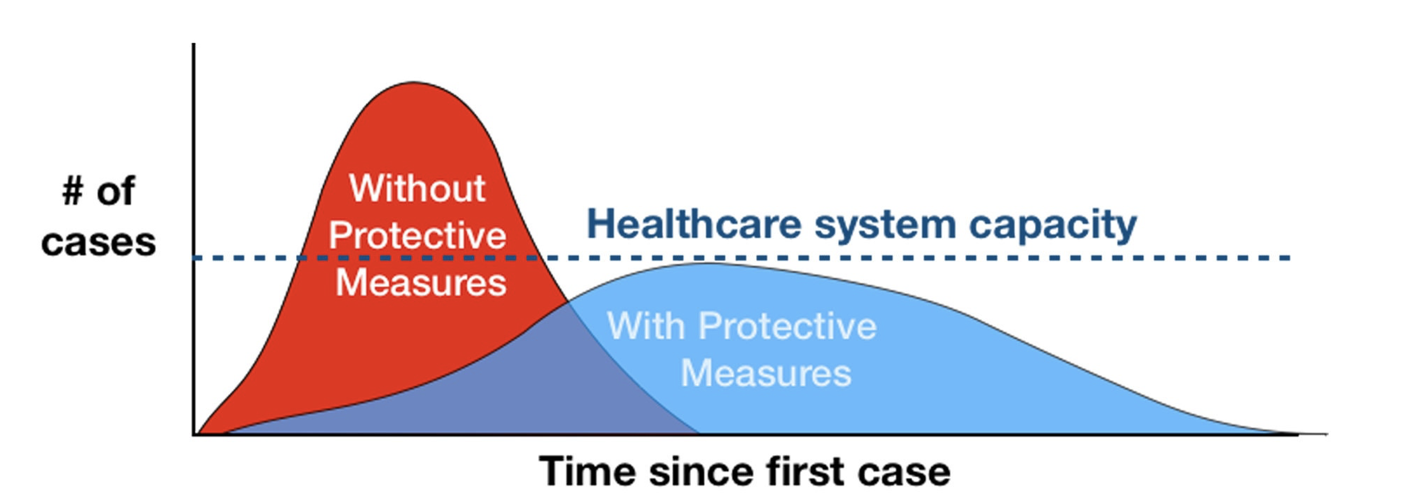
RELATED: Online classes: a protective measure to flatten the curve
Source: CDC/The New York Times
Q: What is the testing process?
DW: The U.S. has the most number of confirmed COVID-19 cases, by far. As of April 8, the country has over 465,000 confirmed cases and about 16,500 confirmed deaths. Obviously, testing has been a critical part of the process.
There are two major ways to test for the novel coronavirus: a molecular test and a serologic antibody test. In essence, the molecular test is able to detect the presence of an active infection, as in the virus is currently in your body. On the other hand, a serologic antibody test, as the name implies, tests for the presence of antibodies in a person’s blood.
Antibodies are produced to help fight off infections and so, a serologic antibody test can tell if a person was infected at some point, not just at the current moment.
If you’re curious to see how exactly both of the tests work, read more down below.
RELATED: What are the different tests for COVID-19 and how do they work?
Q: What state is in more danger for getting the virus?
DW: New York is the current epicenter of the COVID-19 pandemic and as of April 8, the state has over 161,000 confirmed cases of COVID-19 and over 7,000 confirmed deaths. That’s means that one out of every three cases in the U.S. are found in the state of New York. Wild.
The crowded nature of the state, specifically New York City, certainly contributes to the increased likelihood of spreading the virus. New York City has a population of about 8.5 million people with a very high population density. In fact, the city of New York is the most densely populated city in the entire country with over 11,000 people per square kilometer.
Residents of New York City also rely heavily of public transportation and the city is a hotspot for tourists from all over the globe. Taken together, all of these make the state very susceptible to becoming a breeding ground for COVID-19.
Follow Amit Syal on Twitter