A pair of UA researchers recently received a grant to study autoimmune diseases and their precursors.
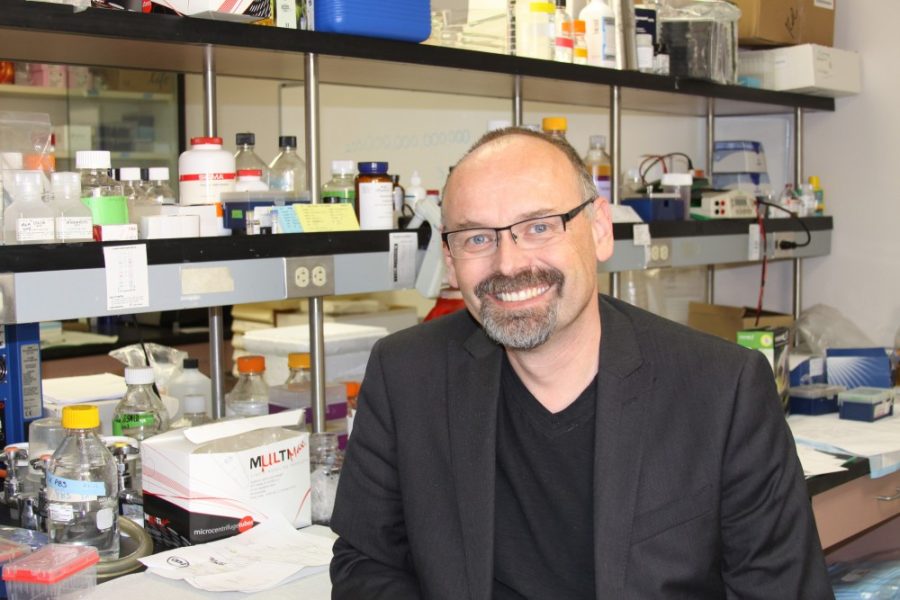
“In very general terms, [autoimmune disease] means that our own immune system turns against our own self, cells and proteins that normally it should be tolerant of,” said Pawel Kiela, UA associate professor in pediatrics, research associate professor in immunobiology and associate professor in physiological sciences.
Kiela and pediatrics department head Dr. Fayez Ghishan will be principal investigators of the five-year, $1.73-million grant from the National Institutes of Health to the UA Steele Children’s Research Center.
Estimates propose that 23 million to 50 million Americans live with an autoimmune disease today. This encompasses over 100 different types of illnesses including inflammatory bowel disease and Crohn’s disease. These diseases occur when immune cells begin to target healthy tissue. By identifying healthy parts of the body as a foreign infection, the body’s own immune system begins killing healthy cells, leading to the deterioration of healthy tissue. This often occurs in the bacteria-rich intestines, but can occur in other parts of the body as well.
RELATED: UA immunologist answers questions on why you should get the flu vaccination
“It’s a complicated matter because there are certain types of autoimmune diseases that are clearly related to genetic predisposition, but we know a lot of it is related to the environment,” Kiela said. “Many autoimmune diseases—inflammatory bowel disease, for example—they hardly exist in underdeveloped countries. But as people immigrate to places like Canada and the U.S. and some European countries, individuals become more susceptible to autoimmune diseases.”
It seems as though the need for a better understanding of autoimmune diseases continues to grow. They’ve been diagnosed more and more within the last 20 years in developing countries as the burden of infectious diseases has lessened, Kiela said.
One of the main issues regarding autoimmune disease is pinpointing why some individuals are susceptible while others are not. Kiela said this involves various factors.
“In general, the factors that are thought to contribute to the rise of autoimmune diseases cannot be explained by genetics alone,” Kiela said. “The lifestyle, the amount of physical activity, the amount of stress, I think all of it contributes.
RELATED: UA researcher wins grant to study cancer and epigenetics
Kiela and Ghishan focused their research on a specific type of immune cell—the dendritic cell, which he called the “sentinel of the immune system.” These cells instruct the immune system to do the opposite of what they’re supposed to do, and that’s not always a bad thing.
“On one hand, they instruct the immune system to develop and maintain tolerance,” Kiela said. “But the very same cells, in a different situation, also promote pathogen destruction. What we focused on in our experiments was a mechanism that signals dendritic cells to remain tolerant.”
Kiela’s primary research has shown promising results in the effort to distinguish what factors can trigger autoimmune disease. He and Ghishan have conducted experiments that expose dendritic cells to different bacterial agents in order to identify which environmental factors change their function. They found that bacterial exposure can promote autoinflammatory reactions in individuals with genetic predispositions and exposure to certain environmental factors.
“[Bacterial exposure] can be distractive in that it can promote autoinflammatory reactions and never be able to stop,” Kiela said. “We’re trying to understand how that happens in dendritic cells.”
The way we currently treat most autoimmune diseases is through immunosuppression, which is essentially weakening the immune system to the point where it cannot kill healthy cells. Unfortunately, this often means the immune system becomes highly susceptible to infection. This type of treatment also greatly increases the risk for cancer.
Kiela and Ghishan hope that their research will lead to better treatments for these afflictions.
“If we are able to identify the entire pathway that leads to this desensitization to transforming growth factor beta, if we know exactly how that happens we may be able to create a pharmacological strategy to prevent that from happening, thus promoting their tolerance,” Kiela said.
Regardless of the specific results of the research, any progress would be beneficial to the fight against autoimmune diseases.
“We hope that if we can find out what happens with dendritic cells,” Kiela said. “This may be either a better solution or possibly an ancillary solution.”
Follow Chandler Donald on Twitter.