Group homes for people with intellectual and developmental disabilities have been one of the hardest hit by this pandemic. The American Association on Intellectual and Developmental Disabilities defines intellectual disability as “a disability characterized by significant limitations in both intellectual functioning and in adaptive behavior, which covers many everyday social and practical skills.”
AAIDD defines developmental disability as “an umbrella term that includes intellectual disability but also includes other disabilities that are apparent during childhood.” Some examples of IDDs include autism spectrum disorders, cerebral palsy, fragile X syndrome and Down syndrome.
There is a variety of housing and residential living situations that people with IDDs and/or their families may choose to get access to extra support and resources. Some people may choose to live by themselves and have direct support professionals to aid them with their daily functions.
RELATED: Nursing homes and assisted living facilities: a battleground for COVID-19
Other people may choose to live in group homes and other community based residential facilities, which typically tend to house 3-6 individuals with IDD and have a supporting staff. These facilities are licensed and receive funding from the state.
Group homes have faced a considerable number of challenges due to the pandemic.
Higher Transmission rates of COVID-19
Residents of group homes and the people who work there have a higher chance of getting infected with COVID-19. An analysis of data reported by group homes in New York State found that the infection rate for people with IDD was around “7,841 per 100,000 for people with IDD compared to 1,910 for New York State.”
While there were limitations to this study, as not all group homes were required to report their numbers to the licensing agency of the region, it still shows the correlation between the group home setting and infection rates.
The author of the study explained in a separate NPR interview that this increase in transmission rate makes sense, given that multiple direct support professionals walk in and out of these group homes and come back to their families.
Residents live in close proximity to each other and some residents need care that does not allow for social distancing. Furthermore, the cancellation of day programs requires staff to spend extra time in these homes. Group homes are taking as many precautions as they can, but it is impossible to completely eliminate increased risk.
Difficulty Explaining the Pandemic to Residents
The coronavirus and the pandemic is quite an abstract concept, and for some residents who have a lower intellectual functioning, they have not been able to completely understand the nature of this pandemic. This especially proved to be a challenge towards the beginning of the pandemic when it came to certain safety precautions like wearing masks as Gina Judy, the chief operations officer of Easterseals Blake Group, said.
“Our individuals had a hard time understanding the facial coverings in particular. We’ve gone to a great length to make these homes feel like their homes. All of a sudden, people are coming into their homes looking like nurses. That was a bit difficult in the beginning,” Judy said.
Judy also emphasized the importance of speaking about the pandemic in a way that is serious but not fear-inducing. It has been a challenge for the residents to adapt. One way that they helped residents understand the importance of wearing masks was by having residents design and create their own masks to wear.
Increased Isolation
The ways in which group homes made it of paramount importance to take extra safety measures to prevent the spread of COVID-19 ended up causing more isolation. Judy said they had to limit the people who could drop in to the group homes, including family members.
“It’s been frustrating for families. They used to be able to just stop by unannounced, but now they have to make arrangements to do zoom calls or phone calls, or arrange for meetings in a park where we can social distance,” Judy said.
Judy also said that some residents had to stop attending their day programs, many of which took place in the community around many people. The increased isolation has been challenging for quite a few of the residents.
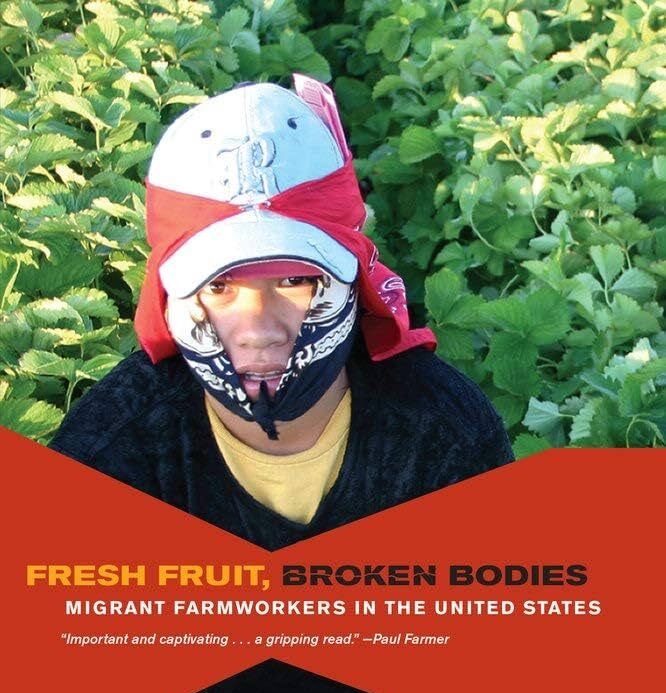
Direct Support Professionals: Heroes putting themselves at risk every day
Direct support professionals are the people who work directly with the residents of group homes and may help residents by verbally prompting them, or may need to provide total physical care for functions like bathing and eating.
Given the nature of their job, these direct support professionals are essential workers who are putting themselves at a higher risk of contracting COVID-19 as they interact with many people and often cannot social distance.
Edwardo Castro, the CEO of the Saguaro Foundation, spoke about how the Saguaro Foundation was having a difficult time and said “all those brave and dedicated employees that took the risk and never once complained — they knew that if they would have quit, there would’ve been no staff. Therefore, it would have been near to impossible to care for our members … This act of valor cannot and will not go unrecognized.”
Direct support professionals, despite facing low wages, overtime hours that may not always be compensated and increased health risks, have continued to work and serve this marginalized and vulnerable community.
How can people help?
Group homes are still in need of all the support they can get. One of the best ways to help out is to just contact and ask them for ways you can be of service.
Judy said that group homes still have a need for cleaning supplies, paper products and personal protective equipment. Although they aren’t doing in-person volunteering, if members of the community have ideas for fun activities that residents can take part in, that is also very much appreciated.
The community was a tremendous help to group homes especially when the pandemic first hit. The IDD community is often overlooked by most, but they are one of the hardest-hit communities. It is imperative that they get support in whatever ways they can.
Follow Udbhav Venkataraman on Twitter