The National Institutes of Health awarded a $1.4 million grant to a team of cardiologists — including two from the UA — last November to study the behavior of a genetic cardiac disease that can cause death in young athletes.
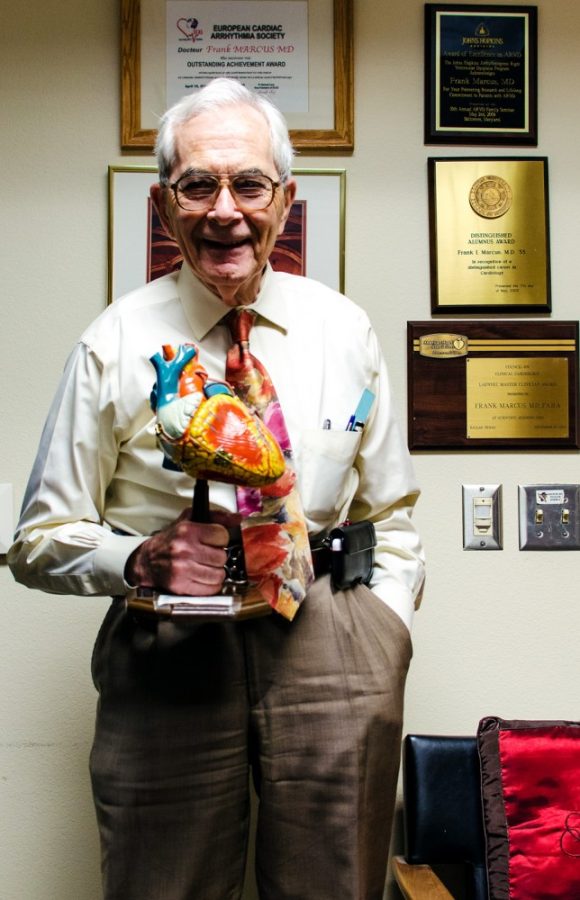
The disease, known as arrhythmogenic right ventricular dysplasia, or ARVD, affects about one in every 5,000 people in the U.S., said UA professor of medicine and co-principal investigator of the study, Dr. Frank Marcus. The exact number of people affected by the disease is unknown.
“The reason it’s hard to know is because you may have the gene but you may feel fine,” Marcus said, “[but] other people can have what seems to be a similar gene and die of the disease.”
ARVD manifests sooner in young athletes, although the reason why is not yet known, said Dr. Julia Indik, a cardiologist and image analyst for the UA research team.
The disease is caused by muscle deterioration in the right side of the heart due to the weakening of cell-to-cell adhesions, Indik said.
The muscle damage causes scar tissue to form in and around the heart, which further increases the heart’s susceptibility to tachycardia, or increased heart rate, Indik said.
Indik said that she is using angiogram analysis, which is a medical imaging technique used to view and study blood vessels, to qualitatively determine to degree of abnormality in ARVD patients.
The study, led by Dr. Jeffrey Towbin from the University of Cincinnati, will also provide diagnostic tests for patients with both right and left ventricular cardiomyopathies.
Part of the grant money will help fund the testing of patients enrolled at 10 health facilities across the nation for functional and structural ventricular abnormalities in their hearts, the results of which will then be reviewed by experts at the participating universities to determine the validity of the ARVD diagnoses, Marcus said.
Multiple labs are contributing to the study, each of which has a specific focus regarding ARVD diagnosis.
The UA lab focuses on angiogram analysis. The other labs involved in the study are researching the genetic component of ARVD by using echocardiogram technology, which uses sound waves to paint a picture of a beating heart.
The UA Sarver Heart Center received $800,000 of the total grant money, said Trina Hughes, the UA study coordinator. Hughes said that part of her job is to compile the UA lab results with those of the other labs across the nation for analysis.
“I’m helping Dr. Marcus connect the dots with all the clinical aspects of the projects,” Hughes said.
Although genetics may hold the key to unraveling the cause of arrhythmogenic ventricular cardiomyopathies, there is still more research to be done, Marcus said.
“Depending on what we find, I think [it is] very likely we or others would be looking to understand why the disease is being caused and then looking [to] either treat or prevent the disease,” Marcus said.