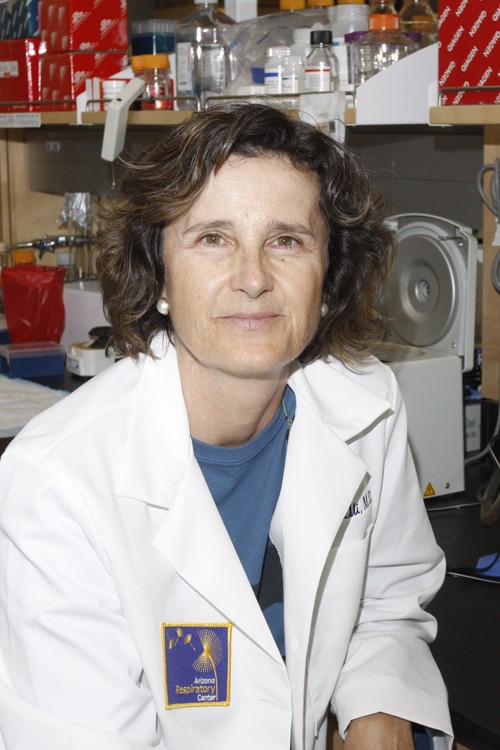
Donata Vercelli is a professor of cell biology and anatomy, the director of the Functional Genomics Laboratory at the Arizona Respiratory Center and the director of the Arizona Initiative for Biology of Complex Diseases, a division of the Arizona Research Laboratories.
She has a degree in medicine from the University of Florence.
After studying in Florence she became a research fellow, then an instructor and an assistant professor in the Division of Immunology at Children’s Hospital/Harvard Medical School. She moved back to Italy briefly before being recruited to UA in 1999. Vercelli sat down with the Daily Wildcat to discuss her research on how domestic dogs affect asthma development.
Daily Wildcat: Can you tell me about the study you are currently working on dealing with the relationship between dogs and asthma?
Donata Vercelli: The principal investigator for the study, on which I am a co-investigator, is Serrine Lau (professor at UA College of Pharmacy). This study was jump-started by another study that suggested that being exposed to dogs, particularly indoor dogs, very early in life might protect from or decrease the risk for asthma.
If you have a dog in the house as a very small child, typically the risk for subsequent asthma is lower. This information is extremely intriguing because it suggests there are some environmental factors that have something to do with protection from asthma. If some environmental factors are identified, it’s possible, in principle, to develop preventive approaches that could limit asthma. This is why the study of environmental factors in asthma (and more generally, in human complex diseases, of which asthma is a prototype) is very important.
The population data seems to suggest that growing up with a dog in the house protects kids from the risk for asthma later in life. Our idea then is to identify the mechanism through which being exposed to a dog early in life turns out to be protective. That’s a way to understand more about the disease and more importantly to develop preventive strategies.
The goal is to find in which way exposure to dogs modifies the plasma protein response in humans in ways that are correlated with asthma. It’s to find the signatures of exposure in the subject’s blood, to try to then correlate these signatures of exposure with the protection to find in which way the early response of the body to the presence of a dog might result in protection from asthma later on, that’s the goal.
You and your colleagues recently received a $937,302 Challenge Grant from The National Institutes of Health. How important is this funding to your research?
It’s exciting, it’s crucial because this is really a pilot study. If we can find evidence that there are modifications in the human proteome, i.e. in the repertoire of proteins people have in their blood, based on exposure to dogs and whether they get asthma later on or not, that allows us to devise studies to answer the really big question: How dog exposure affects asthma.
This study was funded through a mechanism that attracted more than 20,000 applications nationally. Of these 20,000, only approximately three to four percent were funded and our grant was one of them. All together the UA got six of these grants. Our study is one of them.
How long have you been working on this study?
It has been an idea we have had for a while. To pursue this idea, though, we needed to identify colleagues we could work with who could do a high-resolution analysis of blood proteins to really understand and identify signatures of dog exposure. We have identified such a person in Dr. Lau, who is the director of the Southwest Environmental Health Science Center at the UA.
This work will be made possible by longitudinal studies where children enrolled at birth have been followed now up to approximately eight years of age. In the end we know a lot about the children in terms of immune response and respiratory diseases or lack thereof. This was a study initiated by Dr. Halonen and Dr. Wright many years ago. The children have been followed very closely so that we have samples on them, in this case serum samples, and information about their health status or whether or not they are asthmatic at different ages. In this case, whether they have or have not been exposed to dogs in the house. The idea here is to really look at all the proteins in the serum of these children and to identify which of these proteins are different in quality or quantity between groups.
This is something that will be done primarily by Dr. Lau.
Where do you come in on this study?
I come in because this is a typical example of the multi-disciplinary approach to complex diseases I have been championing here at UA for some years. I have brought together different pieces of this puzzle — the respiratory and immunological and proteomics expertise, to study a perfect model of how environmental effects can impact asthma.
The idea here is that complex diseases like asthma are really complex so no individual investigator can have all the expertise necessary to understand them. We have to collaborate with experts complementary to us. The proteomic expertise we don’t have, so we established this with Dr. Lau. We hope by collaborating so closely we will discover what it is that contributes to this protective effect of dog exposure.