With schools set to reopen soon, the unknowing presence of asymptomatic carriers and a high risk of transmission from aerosol could prove detrimental to keeping the spread of disease under control.
A new study out of South Korea published in the Journal of the American Medical Association shows that asymptomatic carriers harbored similar quantities of the novel coronavirus, called a viral load, as those who displayed symptoms.
The study looked at a total of 303 individuals, 193 who were symptomatic and 110 who were initially asymptomatic. However, after isolation, 21 of the 110 initially asymptomatic individuals displayed symptoms, meaning that 89 of the original 303 people never displayed symptoms throughout the entire study.
In other words, the study found that roughly 30% of those infected never develop symptoms yet probably contributed to the spread of infection. This figure matches an estimate from the Centers for Disease Control and Prevention, which estimated that up to 40% of those infected could be asymptomatic earlier in the summer.
RELATED: What are the different tests for COVID-19 and how do they work?
The researchers also found that for those who were asymptomatic, the median time that elapsed from diagnosis to a first negative test was 17 days compared to somewhere between 19 and 20 days for those with symptoms.
The recent change in guidelines from the CDC regarding ending isolation after 10 days, instead of 14, comes from the idea that most of those who are infected stop shedding the virus after a week, even if they still test positive after that time frame.
“Therefore, isolation of infected persons should be performed regardless of symptoms,” the study said. “Because transmission by asymptomatic patients with SARS-CoV-2 may be a key factor in community spread, population-based surveillance and isolation of asymptomatic patients may be required.”
Another study published at the end of July in Nature Research found that aerosols collected in the hospital rooms of COVID-19 patients in Nebraska contained the coronavirus, bolstering a study published in the New England Journal of Medicine in April with similar findings.
“Our results indicate that aerosol and fomite transmission of SARS-CoV-2 is plausible, since the virus can remain viable and infectious in aerosols for hours and on surfaces up to days,” the study in the NEJM said.
RELATED: Maryland-based company generates promising immune response in early trial
In a recent op-ed published in The New York Times called “Yes, the Coronavirus Is in the Air,” Linsey Marr, an engineering professor at Virginia Tech with expertise in airborne transmission of viruses and air quality, argues that aerosol spread of the coronavirus matters more than can be proven yet.
Marr discussed the importance of recognizing aerosol transmission as a contributor to the spread of the virus, citing a plethora of different studies, both peer-reviewed and not.
“I agree that long-range transmission by aerosols probably is not significant, but I believe that, taken together, much of the evidence gathered to date suggests that close-range transmission by aerosols is significant — possibly very significant, and certainly more significant than direct droplet spray,” Marr said in the article.
To help combat COVID-19 spreading through aerosol, there are ventilation products, including a filter based on heated nickel foam, that help neutralize the virus.
A study published in ScienceDirect found that 99.8% of the aerosolized SARS-CoV-2 virus (the virus responsible for COVID-19) and 99.9% of the Bacillus anthracis pathogen (responsible for causing anthrax) were caught and killed by a single pass through a novel nickel foam-based filter when heated up to 200 degrees Celsius.
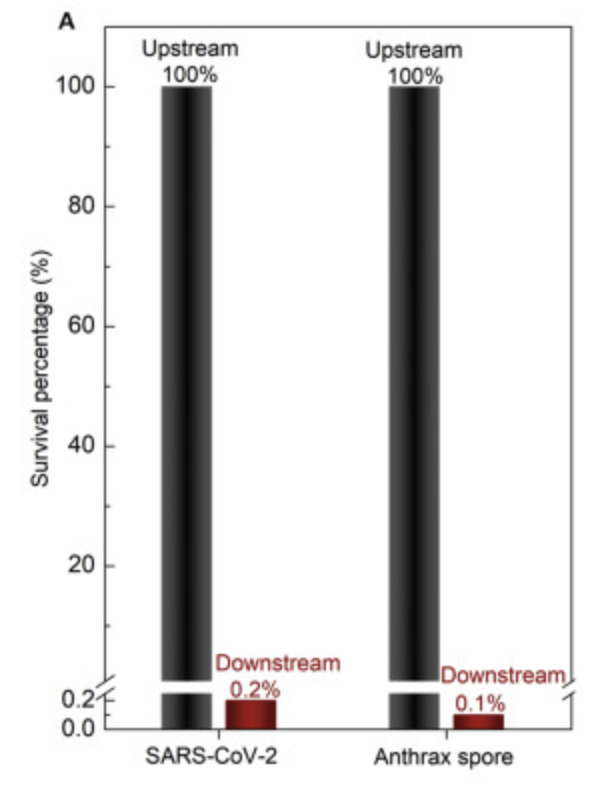
Source: https://doi.org/10.1016/j.mtphys.2020.100249
“So there are products that people are selling and buying in health clubs and other places that ionize the air as it comes through the HVAC system,” said Will Humble, the current executive director for the Arizona Public Health Association. “They claim that it inactivates the virus that would be in that air and therefore lowers the risk.”
Viral transmission via airborne microdroplets is one of the three major modes of transmission of a disease, with the other two being via larger respiratory droplets (coughing, sneezing and talking) and direct contact with contaminated surfaces.
In April, University of Arizona professor and physician Dr. Marvin Slepian submitted three ventilator prototypes for funding by the Department of Defense to address the growing concern of COVID-19. All designs incorporate humidification, temperature control and filtration of expired air to limit infections and contamination risk, according to UA Health Sciences.
With universities on the brink of bringing large crowds back to campus, both asymptomatic carriers of the virus and aerosol transmission further illustrate just how novel this virus and disease are and the desperate need for more aggressive public health measures, such as pooled testing, to help control the spread of the virus.
Follow Amit Syal on Twitter