There are college students everywhere who take 10-15 shots a day. A shot before every meal, a shot in the morning, a shot before bed and more throughout the day. These students need shots for their health, or they can’t handle their day-to-day activity. This is not because they are partying too hard, but because they live with a disease: Type 1 diabetes.
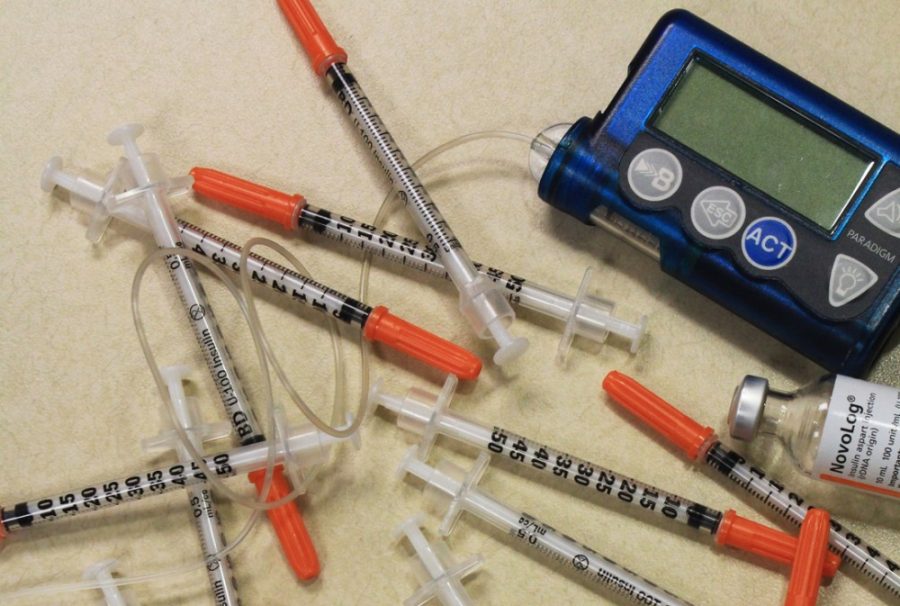
Kelsie Owen, a public health junior, has been a Type 1 diabetic for 18 years. She started out the old-fashioned way with syringes but eventually moved on to an insulin pump when she was 7.
Her mother, Leslie Owen, felt that it was better to switch to the pump. She said she believed it would help manage her diabetes better, and she would be “poked with a syringe less.”
“She was so skinny and had really sensitive skin,” Leslie Owen said, “and she was just getting black and blue and just had sores from where we would do her pokes and give [Kelsie Owen] her insulin shots.”
Since Kelsie Owen was diagnosed young, her mother administered her insulin shots.
“When you think about going into a hospital, your mind tells you that you’ll leave the hospital better, like you [will be] cured or healed, but it was just the beginning,” said Leslie Owen, recalling the day her daughter was diagnosed. “This was the whole start of a lifetime of issues with having to give shots and pokes for her. So, giving her shots was just kind of a whole awareness thing, just to have to do that to your child.”
Diabetes management
Though there is no cure for diabetes, it is a manageable disease. Diabetics must count carbs, monitor blood sugar levels and give insulin accordingly.
DiabeticLink is a website that accommodates Type 1, Type 2 or a prediabetic patients with tools that can help them self-manage their disease. It was started by Hsinchun Chen, director of the Artificial Intelligence Lab at the UA, and Dr. Randall Brown, a physician at University Medical Center who was the medical advisor for the project.
The main goal of the website is to promote patient intelligence, Chen said, so patients can report their status and change their behavior. To help with that, the site has features such as tracking logs, diabetic friendly recipes, restaurant information, social media forums and a risk prediction engine.
“[The risk prediction engine] allows patients to enter their parameters and try to understand their degree of risk of readmissions or other side effects in diabetes,” Chen said.
The risk prediction engine uses over 2,000 patient records to help identify the risk of hospitalization for the patient at hand.
The project was funded by the National Science Foundation and has been active since September 2014. It is free for all users and currently has about 6,000 members. There is also a version in Taiwan, though the U.S. version is more comprehensive, according to Chen.
Lubaina Maimoon, a business graduate student and research assistant at the Artificial Intelligence Lab, said there are many logs for tracking at the same time, including food intake and glucose levels.
“You’re able to see what kind of food would be affecting your glucose levels and at what times,” Maimoon said.
There are also logs for insulin intake, physical activity, HbA1c, blood pressure, cholesterol and weight.
Though the site is catered to diabetics, it is possible for anyone to use the logs. Grace Samtani, a sophomore studying neuroscience and Spanish, research assistant and Type 1 diabetic, said that before they launched the site, many user studies showed that people without diabetes were logging on.
“The family members would go on the website and be like, ‘You know what, I can use this too, because I’m equally affected, and I want to go and help manage my daughter’s condition, my son’s condition, my husband’s or wife’s condition,’” Samtani said. “So, it’s a website that everybody can basically use, because you can track your exercise, you can go to the risk management, and you can predict your risk of stroke or cardiac disease in the next five to 10 years, and everybody can benefit from that.”
Samtani also said DiabeticLink eliminates the need to see a physician every three months if one doesn’t have the means.
“I know that when I was like 5 years old, my parents would keep a manual diary,” Samtani said. “They would write my blood sugars every single day, and [the website] just makes it so much easier. The goal is cyber-enabled patient empowerment, and that’s really what we’re trying to do is empower our patients.”
New technology
Though there are ways to make management easier, doctors and researchers are still finding ways for a Type 1 diabetic to feel less like a pincushion.
Dr. Karen Herbst, an associate professor and endocrinology fellowship director at the UA, said that with a continuous glucose monitor, a Type 1 diabetic only has to check their blood sugar once a day.
“You need to calibrate the meter every day,” Herbst said, “but once it’s calibrated, you don’t need to keep pricking your finger, so it’s once a day.”
Herbst also added that patients have the option of getting a pancreas and kidney transplant that would get rid of their diabetes entirely, though it is not common.
“We actually just had a guy who moved here from Illinois and saw a doctor and immediately got referred to Mayo [Clinic],” Herbst said. “He was deemed to be a really healthy man, and he was in his 60s. I would imagine that if he wasn’t as healthy, they wouldn’t have accepted him.”
Herbst said many people who have Type 1 diabetes get very burnt out from the constant pricking of their skin.
“They prick their finger and then inject themselves with insulin, and then they get low, and then they have to deal with that, and then they might not feel good for the rest of the day,” Herbst said. “I think teenagers get burnt out because they have to work hard and do something at the same time while no one else is doing anything.”
According to the American Diabetes Association, people with Type 1 diabetes are at a higher risk of depression than people without diabetes.
Though Kelsie Owen has been diabetic for most of her life, she said she never felt that it defined her.
“I’ve had diabetes since before I can remember; I don’t remember life without it,” Kelsie Owen said. “Diabetes is a part of my life. It’s not my entire life.”
— Editors note: Joey Fisher, the reporter, is a Type 1 diabetic.
_______________
Follow Joey Fisher on Twitter.