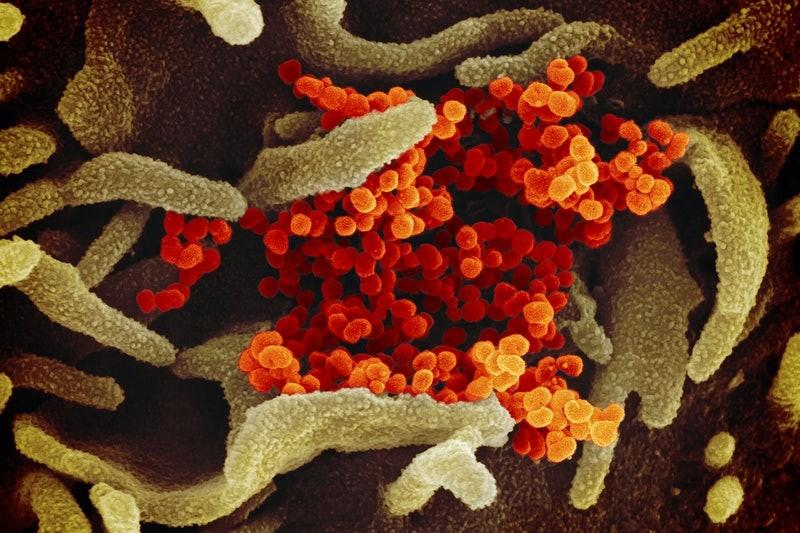
Nursing homes and assisted living facilities: The index case of COVID-19 in the U.S. started here in the state of Washington and to date, these facilities make up a very large percentage of deaths related to COVID-19.
As of May 22, roughly 42% of COVID-19 deaths across the nation have occurred in nursing homes and assisted living facilities, according to The Foundation for Research on Equal Opportunity. In the state of Arizona, over 54% of deaths by COVID-19 have taken place in these facilities. In some states, like Minnesota, this number climbs as high as 81.4%.
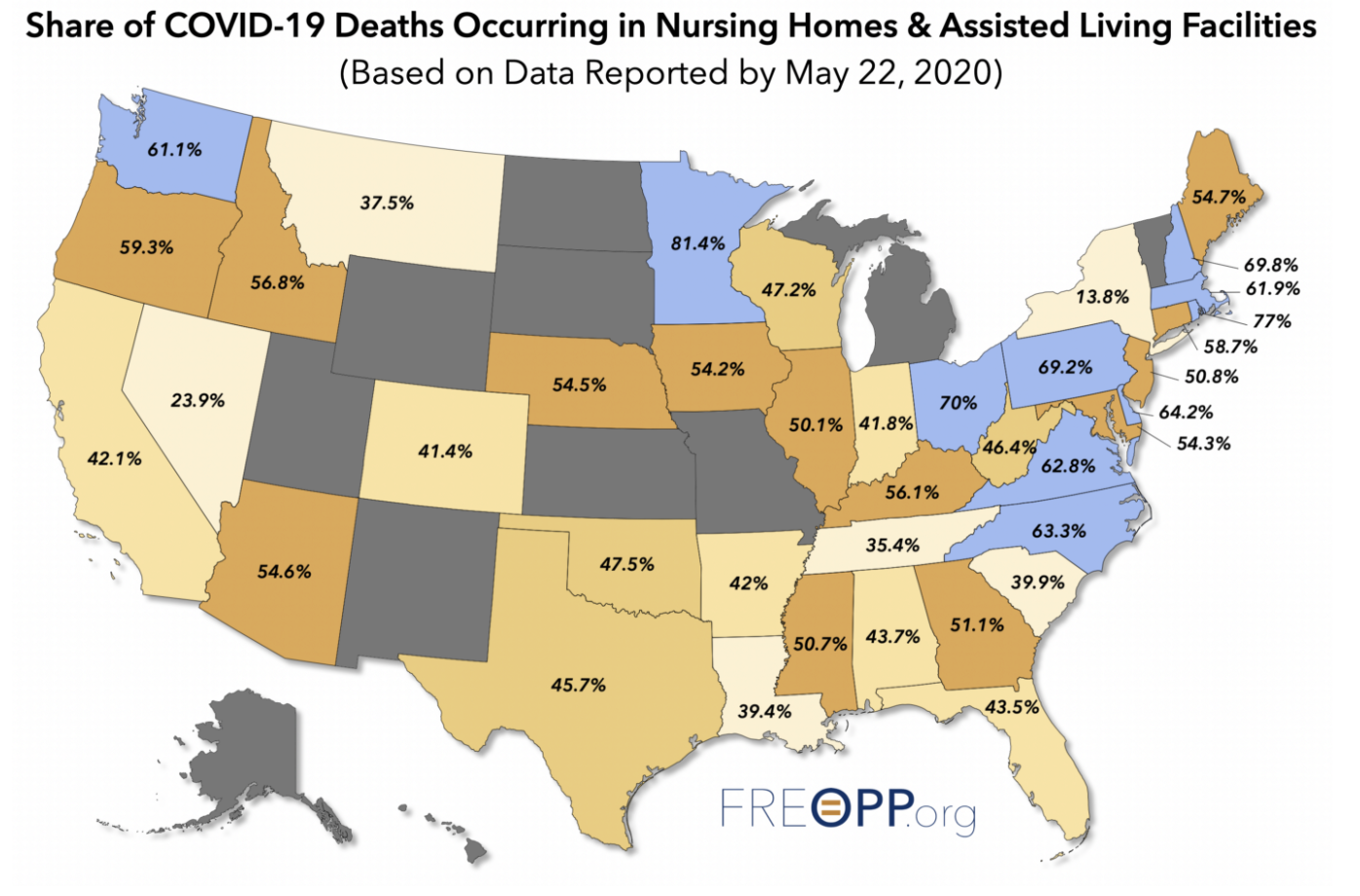
Source: The Foundation for Research on Equal Opportunity
Nursing homes typically house residents who need constant or close to constant medical attention and assistance with activities of daily living, such as bathing, using the bathroom or getting dressed. Assisted living facilities are similar to nursing homes, but they are for residents who don’t need full-time medical attention and typically have more personal space, such as an individual room and bathroom.
The Centers for Disease Control’s most recent estimate for the number of people in nursing homes or residential care communities is around 2.1 million, making up about 0.63% of the U.S. population. So for a group of people who makes up 0.63% of the population, why are they also making up for about 42% of the total COVID-19 deaths?
A typical nursing home, where roughly 1.3 million people in the U.S. reside, is strikingly similar to a university residence hall. We all remember our freshman year dorm setup: a roommate and a community bathroom usually on the ends of the hallway. Well, interestingly enough, nursing homes share a similar layout. Residents have a roommate, usually grouped by the necessity of medical attention, and the pair either shares a bathroom with each other or with the entire hall, which can house upwards of ten residents.
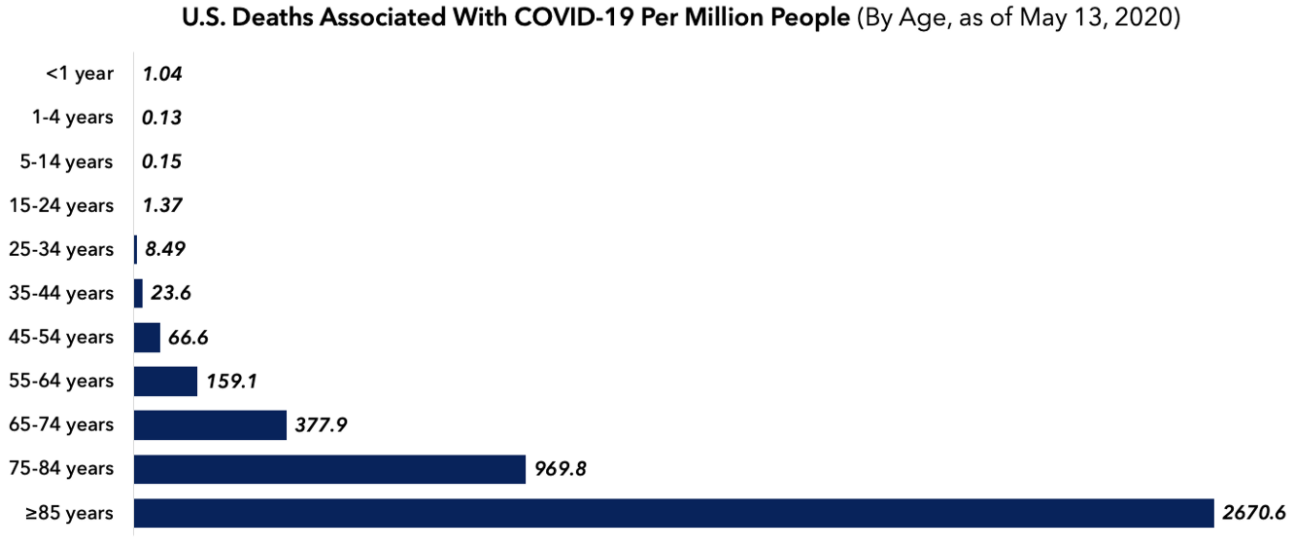
This layout, notably the close proximity of residents to each other, drastically increases the likelihood of transmitting a virus, increasing the total spread of infection and disease prevalence. The more obvious reason for this phenomenon can be explained by the fact that the typical patient in either a nursing home or an assisted living facility is older with underlying health conditions.
When the body is busy dealing with other issues, the odds of having a more severe illness once infected increase drastically since it cannot fight off the virus as well. When looking at nursing homes where the majority of residents need serious medical attention, a patient there would not fare well given an unfortunate combination of old age and poor health.
Source: The Foundation for Research on Equal Opportunity
This trend of nursing homes and assisted living facilities is not limited to just the U.S.
“[T]he % of COVID-related deaths among care home residents ranges from 19% in Hungary to 62% in Canada,” when looking at nine countries: Belgium, Canada, Denmark, France, Germany, Hungary, Ireland, Israel and Norway, according to International Long Term Care Policy Network.
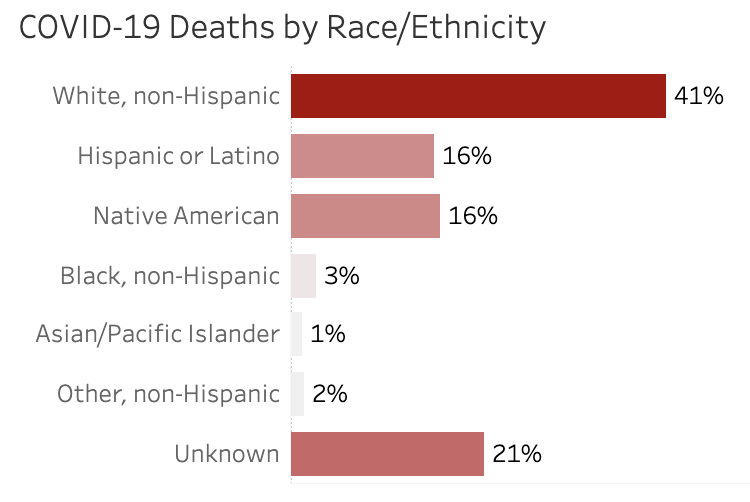
We’ve seen before that this global pandemic has exposed long-standing discrepancies in not only our healthcare system but also in the health of our citizens of differing races.
RELATED: COVID-19 death rate potentially lower, disproportionately affects minority groups
Minority groups, such as African Americans or Native Americans, have been hit disproportionately harder these past few months. However, a significant difference based on residential location within a city is without a doubt easier to combat.
Source: Arizona Department of Health Services
As of May 27, the U.S. has over 1.7 million confirmed cases of COVID-19 and recently passed a grim benchmark of 100,000 deaths. As pretty much every state is now partially opened, more restrictions on nursing homes and assisted living facilities must be put into place in order to avoid an even greater dichotomy of the percentage of deaths coming from these facilities versus those from the rest of the population.
Follow Amit Syal on Twitter