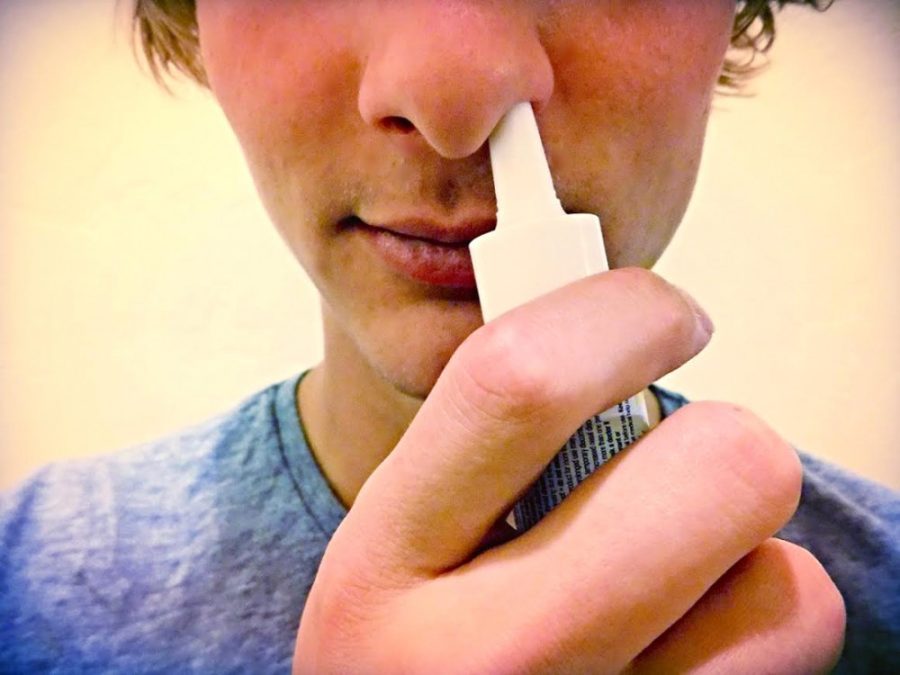
UA assistant psychology professor Mary-Frances O’Connor is using oxytocin nasal spray to further understand the physiological mechanisms behind complicated grief.
“Oxytocin is a hormone in the body that is very much related to how we bond to other people,” O’Connor explained. “This is true in animals, nursing mothers or romantic bonding. It occurred to me that this may be a hormone system in the body that is operating differently in people that have complicated grief.”
Approximately 10 to 20 percent of people develop complicated grief and experience emotional pain, intense yearning and difficulty performing normal daily functions long after the passing of their loved one, according to O’Connor. This condition is also associated with increased morbidity and mortality.
“Most people, when they lose a loved one, are resilient,” O’Connor said. “It is very distressing and emotional, but most people can adapt and recover. However, there is a small group of people that, when they lose a loved one, they cannot ever really adapt. This is called complicated grief.”
O’Connor’s prior research shows that the part of the brain that seems uniquely activated in complicated grief is an area called the nucleus accumbens. It is a part of the reward network in the brain that is responsible for positive emotions when spending time with loved ones and feelings of sadness during separation. This area of the brain is known to hold many neurons with receptors for the neuropeptide hormone oxytocin.
O’Connor hypothesizes that abnormally low levels of oxytocin bound to receptors in the nucleus accumbens during bereavement may be responsible for the development of complicated grief. Functional magnetic resonance imaging will be performed on 40 adults with complicated grief to discover if the nucleus accumbens region is disregulated by measuring blood flow in the brain.
“The fMRI tool allows us to measure changes in blood flow in the brain,” said Brian Arizmendi, a UA clinical psychology graduate student working with O’Connor. “Those areas where we measure increased blood flow are receiving an abundance of oxygen necessary for brain activity. Thus we measure blood flow as an accurate, albeit indirect, measure of brain activity in what is known as Blood Oxygen Level Dependent signal.”
fMRI imaging will be done twice: once after the oxytocin nasal spray, and once after the saline spray to act as a control condition. Then, fMRI images will be collected while participants will be asked to focus on their emotional experience while viewing an image of their deceased loved one during the scan.
According to O’Connor, by comparing the images of administering oxytocin versus saline, it can be determined which neuronal receptors are already full or activated. This will indicate whether or not the oxytocin receptor system is in fact the one affected as opposed to a different receptor system, such as dopamine.
Because oxytocin only has a half-life of 20 to 30 minutes, O’Connor said she does not think that the hormone can serve as a pharmacologic treatment for complicated grief. However, both O’Connor and Arizmendi are hopeful that the study will uncover the differences between those with and without complicated grief and how to better treat the condition.
“Individuals in the U.S. are living longer than ever before, resulting in an ever-increasing number of bereavement experiences,” Arizmendi said. “It is our hope that data from this study will significantly add to our understanding of the biological and neural mechanisms behind complicated grief, which may pave the way for improved treatment for those with this debilitating condition.”
_______________
Follow Kimberlie Wang on Twitter.