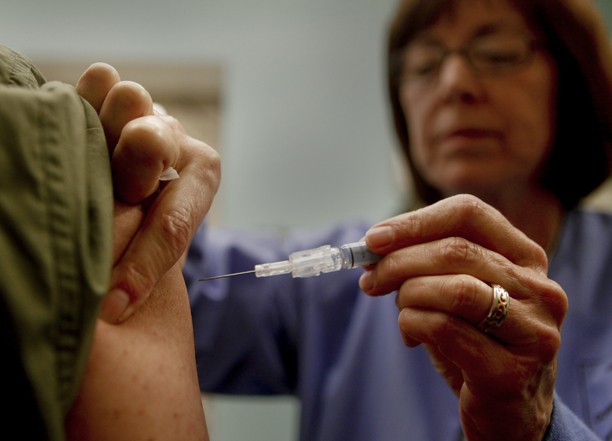
Among the long list of reasons the fearful give for why they’re not getting a flu shot — hatred of needles, skepticism about vaccines, laziness — there’s one that relates more closely to economics: cost. For while doctors urge everyone to get the vaccine, flu shots, like many other things in life, are not free. Stop by your local drugstore and you’ll shell out $30 or so for the pleasure of getting poked by a needle behind a suggestion of a curtain.
So why aren’t flu shots free, or nearly free? After all, they’ve been around for a while and there’s a lot of demand. Isn’t it about time flu shots cost the same as, say, generic Tylenol?
If only, says Curtis Allen, a spokesman for the Centers for Disease Control and Prevention. The real question should probably be, why does the flu shot cost so little?
That’s because the process of manufacturing and distributing the flu shot is a huge headache for pharmaceutical companies. The influenza vaccine must be made anew each year, beginning in February. Researchers determine what strains to put in the vaccine after looking closely at what types of flu are most prevalent in the Southern Hemisphere throughout its winter, which is the Northern Hemisphere’s summer.
Then the handful of pharmaceutical companies that make the vaccine have to estimate how many doses to make. Make too many, and they’ll have to throw away a bunch if people don’t get the flu shot; make too few, and they’ll cause a panic about vaccine shortages.
Vaccines for other illnesses, such as measles, mumps and rubella, can be used until their expiration date, which is often years after they’re made. Influenza vaccines are usually only used September through January and then go in the trash. And there are no regulations saying people have to get flu vaccines, meaning it’s very difficult for companies to estimate how many they should make.
“It can be a risky business,” Allen said. “They have to make a decision on the number of doses to make many, many months before the flu season actually happens.”
This year, companies have produced about 145 million doses, he said. Only about 129 million have been distributed. Last year, companies lost even more on the flu vaccine because it was such a light flu season and fewer people decided to get the shot. Only about 42 percent of the U.S. population got an influenza vaccine last year, which meant that about 30 million doses were never used and had to be destroyed.
“One of the primary challenges for influenza vaccines production is gauging the demand for [the] vaccine,” said Donna Cary, a spokeswoman for Sanofi Pasteur, one of the companies that makes the influenza vaccine. “The single most important thing a person can do to help protect themselves against influenza and to ensure that vaccine will be available for them next year … is to get an annual flu shot so that vaccine supply and demand are more closely aligned.”
Influenza vaccines cost health care providers from $10 to $16 per dose, according to the CDC. They’re by far the cheapest vaccine on the list. The tetanus vaccine costs a provider $38, human papillomavirus vaccine is $130 and Hepatitis B vaccine is $52.