As every day passes, the idea of containing the coronavirus gets exponentially further and further away. Literally.
RELATED: Online classes: a protective measure to flatten the curve
What started out as a breakout in one country has turned into a pandemic that has taken the lives of well over 11,000 people across the globe.
In its early stages, COVID-19 was often compared to the influenza virus that takes hundreds of thousands of lives around the globe each flu season. The SARS-CoV-2 virus has taken the world by storm and by surprise, no doubt about it.
The U.S. healthcare system is on the brink of being overwhelmed to the point where the idea of using bandanas and reusing masks for sick patients are being talked about. Crazy, huh?
Herd immunity is a phenomenon that becomes relevant every flu season. But what exactly is it?
In essence, this phenomenon describes the idea that when enough people in a given community have immunity to a given virus — whether it be influenza or SARS-CoV-2 — then the rest of the population becomes a lot less susceptible to becoming infected.
As a consequence of herd immunity, the herd effect is the decrease in infection rate in the part of the community that is not immune to the virus.
Typically with the influenza virus, herd immunity arises when people take advantage of the ever-useful vaccine and mitigate the risk of those people who can’t become vaccinated of becoming ill with the flu. There’s an issue with COVID-19: there is no vaccine out yet.
In theory, if enough people become infected with the SARS-CoV-2 virus, then herd immunity could arise, just in a very atypical fashion. This is obviously a side effect, since no one is trying to artificially create a pandemic. At least we’d hope so.
Experts typically recognize that the manner by which herd immunity arises isn’t the deciding factor, but just that a certain percentage of the population becomes immune. The percentage required to achieve herd immunity varies greatly between different viruses. Typically, at least 60% is the bare minimum for the most viruses that needs to be achieved before herd immunity can become a possibility.
When dealing with viruses, the R0 is the basic reproduction number and it describes how many other people will get infected from any one individual who has contracted the disease. Experts typically place the R0 value of COVID-19 between 2-3, meaning that 2-3 other people will contract COVID-19 from an individual who is sick. This places the percentage of the population required for herd immunity (H) between 50% and 67%. But given the unpredictable nature of the virus, that’s likely to change.
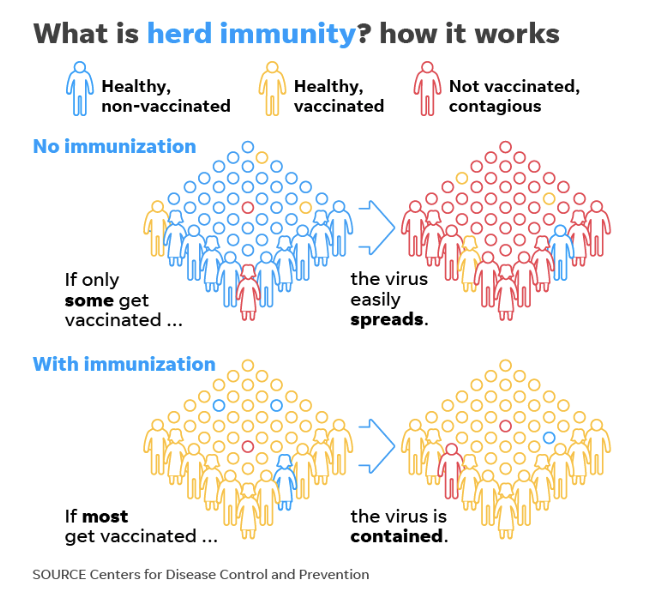
Source: CDC
The main difference between immunity that comes from a vaccine or being infected by Mother Nature is the efficacy. Vaccinations are an active, artificial manner of immunity that helps someone person deal with the virus, while infections are ultimately the most natural way to provide immunity.
Although both types of immunity last for a very long time, a natural form of immunity is typically more effective and is able to elicit more antibody production, which helps for a possible future infection.
With the possibility a winter resurgence of COVID-19, herd immunity could help to mitigate the dangerous effects later on this year. However, with its current state of mitigation, the virus seems unstoppable.
Researchers around the world are working on creating a vaccine against the SARS-CoV-2 virus and, knowing the efficacy of the influenza vaccine, it would be inane to not take advantage of the new vaccine — granted it’s FDA approved and gone through a series of clinical trials.
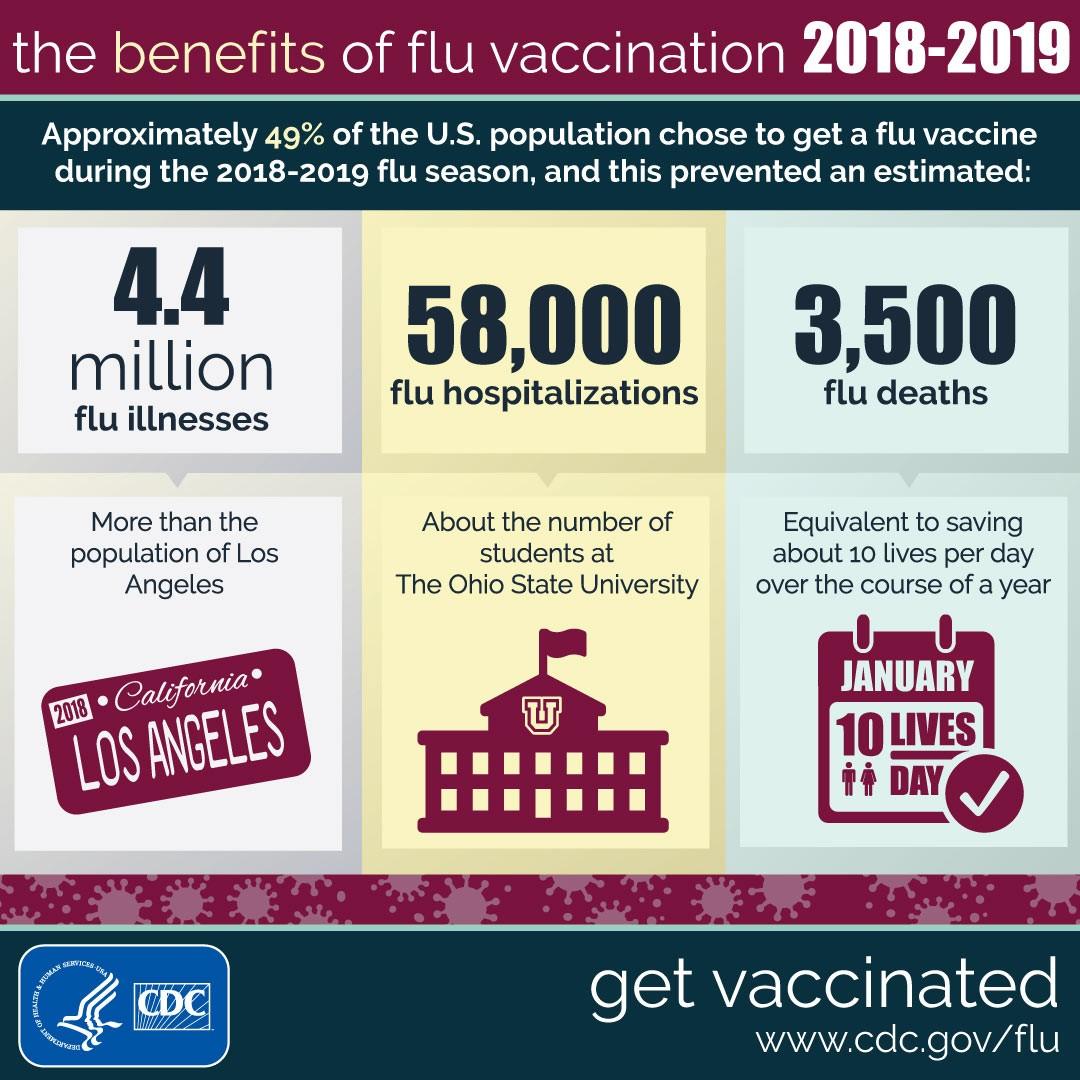
Source: CDC
The Government has been discussing possible ways to tackle the “invisible enemy.” The chief science officer of the UK government, Patrick Vallance, indicated that the country’s aim could potentially be the create herd immunity by letting the virus run its course to reach the 60% value.
If a vaccine isn’t created in the near future, it seems like herd immunity will be the way that we see an eventual decrease in the number of cases per day. However, if we rely on herd immunity, then our curve can be astronomically high and we run the risk of the U.S. healthcare system becoming severely overwhelmed with very sick patients.
So, how do we create herd immunity? Do we let people get sick and let Mother Nature run its course? If a vaccine can be put out in a short enough time, it is undoubtedly the better way to achieve herd immunity. But given the unlikely nature of that, only time will tell what will happen.
Follow Amit Syal on Twitter